1. Introduction
Gabapin, containing the active ingredient Gabapentin, is a widely prescribed anticonvulsant and neuropathic pain modulator. It is primarily utilized in the management of seizures and nerve-related pain disorders. Originally developed to mimic the neurotransmitter GABA, Gabapentin functions differently, offering a unique therapeutic profile that has transformed the management of chronic neurological and pain conditions.
Pharmacologically, Gabapin is categorized as an anticonvulsant and analgesic adjuvant. Its introduction into clinical use followed rigorous evaluation, with the U.S. FDA approving Gabapentin in 1993 for partial seizures. Over time, its efficacy in treating neuropathic pain expanded its therapeutic scope, leading to off-label applications across multiple chronic pain syndromes and psychiatric conditions.
Today, Gabapin remains integral to the treatment of epilepsy, postherpetic neuralgia, and diabetic neuropathy, enhancing quality of life through effective nerve pain control and seizure prevention.
2. Composition and Formulation
The principal active compound in Gabapin is Gabapentin, a structural analogue of gamma-aminobutyric acid (GABA). Although it resembles GABA chemically, it does not act directly on GABA receptors. Instead, it modulates calcium channel activity within the central nervous system.
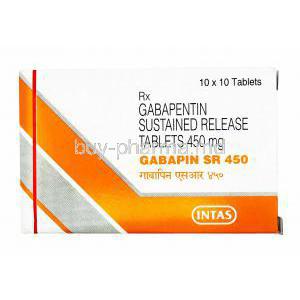
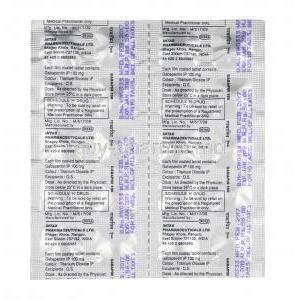
- Dosage forms: Capsules, tablets, and oral solution.
- Strengths available: 100 mg, 300 mg, 400 mg, 600 mg, and 800 mg.
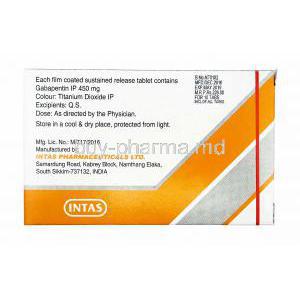
- Excipients: Lactose monohydrate, magnesium stearate, and gelatin (capsule shell) to maintain stability and bioavailability.
Each formulation is designed to ensure consistent absorption and efficacy, offering flexibility across a range of therapeutic needs.
3. Mechanism of Action – How Gabapin Works
Gabapin exerts its pharmacologic activity through modulation of voltage-gated calcium channels located in presynaptic neurons. By binding to the α2δ subunit of these channels, Gabapentin reduces calcium influx during neuronal excitation.
This modulation results in diminished release of key excitatory neurotransmitters such as glutamate, noradrenaline, and substance P. The outcome is a notable reduction in neuropathic pain signaling and neuronal hyperexcitability.
Unlike classic anticonvulsants, Gabapin’s mechanism is non-GABAergic—it neither enhances GABA synthesis nor binds to GABA receptors. This distinct mode of action contributes to its favorable safety profile and wide therapeutic acceptance.
4. Medical Uses and Indications
4.1 Approved Uses
- Partial Seizures: Used as adjunctive therapy in adults and children, with or without secondary generalization.
- Postherpetic Neuralgia: Effective in alleviating nerve pain following shingles infection.
- Diabetic Neuropathy: Provides relief from chronic burning or tingling sensations in diabetic patients.
4.2 Off-Label Uses
- Restless Legs Syndrome (RLS): Reduces limb discomfort and improves sleep quality.
- Fibromyalgia: Eases widespread musculoskeletal pain and fatigue.
- Anxiety Disorders: Demonstrates anxiolytic effects in generalized anxiety and social phobia.
- Migraine Prophylaxis: Reduces attack frequency and intensity in some patients.
- Alcohol Withdrawal: Supports detoxification and reduces withdrawal-related symptoms.
- Trigeminal Neuralgia: Relieves stabbing facial pain unresponsive to other agents.
5. Dosage and Administration
5.1 Recommended Dosage Ranges
For epilepsy, the typical starting dose is 300 mg once daily, titrated up to 900–1800 mg per day, divided into three doses. In neuropathic pain, doses usually range between 900–2400 mg daily, depending on tolerance and response.
5.2 Titration and Adjustment Guidelines
Gradual titration minimizes adverse effects such as dizziness and somnolence. Dose increments should not exceed 300 mg per day. In patients with renal impairment, dosage adjustments are mandatory to prevent accumulation and toxicity.
5.3 Administration Instructions
- Can be taken with or without food.
- Maintain consistent dosing intervals for optimal therapeutic levels.
- In case of a missed dose, take it as soon as remembered, unless it is near the next scheduled dose.
6. Warnings and Precautions
Gabapin should be administered with vigilance due to its influence on mood and neurological activity. Patients should be monitored for signs of suicidal ideation, agitation, or unusual behavior.
- CNS Effects: Drowsiness, dizziness, and impaired coordination are common and may affect activities requiring alertness.
- Discontinuation: Abrupt withdrawal may precipitate seizures; taper gradually under supervision.
- Dependence Potential: Long-term misuse can lead to physical dependence in vulnerable individuals.
7. Contraindications
- Known hypersensitivity to Gabapentin or any component of the formulation.
- Severe renal impairment when dosage is not properly adjusted.
- Patients with chronic respiratory depression or concurrent use of strong CNS depressants.
8. Careful Administration and Monitoring
Regular clinical monitoring is essential, particularly in patients with existing comorbidities.
- Renal and Hepatic Impairment: Require dosage modification and periodic assessment of organ function.
- Psychiatric Conditions: Evaluate for depressive symptoms or behavioral changes.
- Polypharmacy: Use caution in patients concurrently taking opioids or sedatives.
9. Drug Interactions
Gabapin exhibits minimal pharmacokinetic interactions but requires awareness of certain combinations.
- Opioids: Increased risk of respiratory depression and sedation when co-administered with morphine or oxycodone.
- Antacids (Aluminum or Magnesium-based): Can decrease Gabapentin absorption; separate doses by at least two hours.
- Alcohol and CNS Depressants: Additive drowsiness and cognitive impairment may occur.
- Antiepileptics: Minimal interference with phenytoin, carbamazepine, or valproate, ensuring flexible combination therapy.
Gabapin stands as a cornerstone therapy for neuropathic pain and seizure management, balancing efficacy with a favorable safety margin when used judiciously under medical guidance.
10. Side Effects
10.1 Common Side Effects
Gabapin (Gabapentin) is generally well tolerated; however, certain side effects may emerge during therapy. The most frequently observed are related to the central nervous system and metabolic balance. These effects often diminish as the body adapts to the medication.
- Dizziness and Drowsiness: Transient lightheadedness and somnolence are common, particularly at therapy initiation or dose escalation.
- Ataxia: Impaired coordination or unsteady gait may occur in some patients, especially at higher doses.
- Peripheral Edema and Weight Gain: Fluid retention, particularly in the lower limbs, may contribute to mild swelling or gradual weight increase.
- Gastrointestinal Disturbances: Nausea, dry mouth, and fatigue are occasional complaints, often mitigated by taking the medication with food.
- Visual Disturbances: Blurred or double vision may appear temporarily due to altered neural transmission within the visual cortex.
10.2 Serious Adverse Effects
Though rare, serious reactions demand immediate medical attention. These adverse events may indicate systemic hypersensitivity or central nervous complications.
- Suicidal Ideation and Behavioral Changes: Mood swings, anxiety, or self-harm thoughts can develop in susceptible individuals; early detection is crucial.
- Hypersensitivity Reactions: Severe skin rashes, angioedema, or anaphylaxis have been documented; prompt discontinuation is essential in such cases.
- Respiratory Depression: When used with opioids or other CNS depressants, Gabapin can cause slowed breathing, necessitating close observation.
- Withdrawal Symptoms: Sudden cessation may trigger insomnia, anxiety, or rebound seizures—gradual tapering is imperative to avoid adverse rebound effects.
11. Administration in Special Populations
11.1 Elderly Patients
In geriatric populations, pharmacokinetics are influenced by reduced renal clearance and altered drug metabolism. Careful dose titration minimizes side effects such as sedation and balance impairment.
- Start with the lowest possible dose and increase gradually.
- Frequent renal function assessment is advised to prevent accumulation.
- Increased vigilance for dizziness or falls is required, as these can lead to fractures or injury.
11.2 Pregnant Women and Nursing Mothers
Gabapin falls under Pregnancy Category C, indicating potential risks that must be weighed against therapeutic benefits. Animal studies have shown adverse fetal effects, though controlled human studies are limited.
- Prescribe only when potential maternal benefits outweigh fetal risks.
- Newborns exposed in utero may experience withdrawal or respiratory complications post-delivery.
- Gabapentin is excreted in breast milk; infants should be monitored for drowsiness or feeding difficulties during lactation.
11.3 Pediatric Administration
Gabapin demonstrates proven efficacy in children aged three years and older with partial seizures. Pediatric dosing must consider body weight and clinical response to ensure safety and effectiveness.
- Children typically require 10–15 mg/kg/day, divided into three doses.
- Gradual titration reduces risk of sedation or behavioral changes.
- Limited data exist for non-epileptic pediatric use; such cases require specialist supervision.
12. Overdosage
Excessive ingestion of Gabapin may lead to neurological and gastrointestinal symptoms. While fatalities are rare, emergency intervention is warranted in severe cases.
- Symptoms: Double vision, slurred speech, profound drowsiness, lethargy, and diarrhea are typical manifestations.
- Management: Treatment is supportive—airway maintenance, hydration, and vital monitoring form the cornerstone of care.
- Hemodialysis: Effective in removing Gabapentin from circulation, particularly in patients with renal impairment or severe toxicity.
13. Storage and Handling Precautions
Proper storage maintains the medication’s potency and ensures patient safety.
- Store below 25°C, in a dry, cool location away from direct sunlight.
- Keep out of reach of children and pets to prevent accidental ingestion.
- Do not use beyond the expiration date. Dispose of unused capsules safely through authorized medical waste systems.
14. Patient Counseling and Important Advice
Patient education plays an integral role in successful Gabapin therapy. Understanding proper administration and recognizing warning signs enhances both safety and therapeutic outcomes.
- Dosage adjustments should always be gradual; never discontinue abruptly.
- Avoid alcohol, sedatives, or hazardous activities until the body’s reaction to the drug is understood.
- Adherence to dosing schedules is vital for sustained seizure control and nerve pain relief.
- Report any signs of mood alteration, anxiety, or suicidal ideation immediately to a healthcare provider.
15. Summary of Key Takeaways
Gabapin (Gabapentin) stands as a multifunctional agent with proven benefits in epilepsy and neuropathic pain. Its flexibility across diverse neurological disorders underscores its therapeutic significance. When administered judiciously, Gabapin offers profound symptom relief with manageable side effects.
- Individualized dosing ensures optimal efficacy and minimizes adverse effects.
- Regular monitoring enhances patient safety, particularly in elderly and special populations.
- Its off-label benefits—ranging from fibromyalgia to anxiety—highlight its versatility in modern clinical practice.
Through responsible use, careful titration, and adherence to medical supervision, Gabapin remains a cornerstone in the management of chronic pain and seizure disorders.
Gabapin, Gabapentin Capsule FAQ
- What should I avoid while taking gabapentin?
- Does gabapentin help you sleep?
- What organ is gabapentin bad for?
- What are the positive effects of gabapentin?
- Is gabapentin a muscle relaxer?
- What kind of pain is gabapentin best for?
- Who cannot take gabapentin?
- Does gabapentin make you sleepy?
- What are the permanent side effects of gabapentin?
- How long before bed should I take gabapentin?
- What happens if you suddenly stop gabapentin?
- Does gabapentin really stop nerve pain?
- Does nerve pain get worse after stopping gabapentin?
- Can gabapentin make nerve pain go away?
- Should you drink a lot of water with gabapentin?
- Can I take vitamin D with gabapentin?
- Which is stronger, tramadol or gabapentin?
- How quickly does gabapentin start working?
- What is better, pregabalin or gabapentin?
- What is the biggest side effect of gabapentin?
- How quickly does gabapentin make you sleepy?
- Can gabapentin cause memory loss?
- Why do I feel so good on gabapentin?
- Does gabapentin affect blood pressure?
- Does memory come back after stopping gabapentin?
- Why do most people take gabapentin?
- Does gabapentin cause you to pee more?
What should I avoid while taking gabapentin?
- Strong painkillers—morphine being an example—often leave you feeling profoundly sleepy and a touch light‑headed, especially once gabapentin is introduced.
- Antidepressants, such as amitriptyline or fluoxetine, represent a group.
- Antipsychotic medicines, used for mental‑health conditions, like schizophrenia or bipolar disorder
Does gabapentin help you sleep?
Yes
What organ is gabapentin bad for?
- Kidney
- Heart
What are the positive effects of gabapentin?
Initially prescribed to manage epilepsy and the nerve pain that follows conditions such as shingles, the medication soon revealed a calming effect in a number of patients. Observing this clinicians began to use it off‑label for a range of issues including anxiety, restless‑leg syndrome and even alcohol‑withdrawal symptoms.
Is gabapentin a muscle relaxer?
Gabapentin first entered the pharmacopeia as a drug meant to relax muscles and suppress spasms.
What kind of pain is gabapentin best for?
Nerve pain
Who cannot take gabapentin?
- Any history of medication misuse or dependence.
- Any attempt to become pregnant or an existing pregnancy.
- Any sodium‑ or potassium‑restricted diet or kidneys that are not functioning properly (gabapentin liquid contains sodium and potassium so consult a physician before taking it).
Does gabapentin make you sleepy?
Yes
What are the permanent side effects of gabapentin?
- Mood swings
- Shift in behavior
- Depressive episodes
- Anxiety
- Memory lapses
- Weakened muscles
How long before bed should I take gabapentin?
30 minutes
What happens if you suddenly stop gabapentin?
- Withdrawal signs may appear as early as twelve hours after the medication is stopped. They can be delayed until up to a week later, and the episode can linger for roughly ten days. The typical effect of gabapentin withdrawal includes nausea, dizziness, headaches, sleeplessness, and anxiety.
Does gabapentin really stop nerve pain?
Yes
Does nerve pain get worse after stopping gabapentin?
Yes
Can gabapentin make nerve pain go away?
No
Should you drink a lot of water with gabapentin?
Yes
Can I take vitamin D with gabapentin?
Yes
Which is stronger, tramadol or gabapentin?
Tramadol tends to be the go‑to for pain, whereas gabapentin usually proves more effective for the lingering ache of chronic nerve damage.
How quickly does gabapentin start working?
1 week
What is better, pregabalin or gabapentin?
Gabapentin’s efficacy tends to outstrip that of pregabalin at dosing levels.
What is the biggest side effect of gabapentin?
Dizziness
How quickly does gabapentin make you sleepy?
2-3 hours
Can gabapentin cause memory loss?
Yes
Why do I feel so good on gabapentin?
Gabapentin works by standing in for GABA, the brain’s calming neurotransmitter. When GABA’s soothing influence is disrupted, it has been linked to a range of mental‑health issues, including panic disorder and depression.
Does gabapentin affect blood pressure?
Yes
Does memory come back after stopping gabapentin?
Yes
Why do most people take gabapentin?
- Gabapentin is employed to stave off and tame seizures for adults as well as children from the age of three onward. Moreover, it serves to soothe the lingering nerve pain that can arise after a shingles episode in adult patients.
Does gabapentin cause you to pee more?
Yes