Introduction to Torsemide Injection
Overview of Torsemide as a Loop Diuretic
Torsemide is a potent loop diuretic, belonging to the sulfonylurea class, widely employed in the management of fluid overload. Its primary function is to induce diuresis by inhibiting sodium and chloride reabsorption in the thick ascending limb of the loop of Henle. This pharmacologic action promotes significant fluid loss, making it invaluable in the treatment of conditions marked by volume excess.
Injectable Form: Clinical Relevance and Usage Settings
Torsemide Injection serves as a critical intervention in acute care settings where oral administration is impractical. It is commonly administered in emergency departments, intensive care units, and perioperative environments. The parenteral form allows for rapid diuretic onset, making it the formulation of choice for patients experiencing acute decompensation or those with compromised gastrointestinal absorption.
Regulatory Approval and Global Availability
Torsemide Injection is approved by regulatory authorities in multiple regions including the FDA (United States), EMA (Europe), and PMDA (Japan). It is available globally under various brand and generic names, ensuring broad accessibility in both hospital and outpatient settings.
Mechanism of Action: How Torsemide Injection Works
Inhibition of Na⁺/K⁺/2Cl⁻ Co-Transporter in the Loop of Henle
Torsemide inhibits the Na⁺/K⁺/2Cl⁻ symporter located in the thick ascending limb of the loop of Henle. This blockade impairs the reabsorption of sodium, potassium, and chloride ions, thereby increasing solute and water excretion. The result is potent natriuresis and subsequent reduction in plasma volume.
Onset of Action and Peak Effects
When administered intravenously, torsemide begins to act within 5 to 10 minutes. Peak diuretic effects are typically observed within 30 minutes. The duration of action ranges between 4 to 6 hours, allowing for flexible dose titration based on patient response.
Pharmacokinetics and Bioavailability in IV Form
The IV formulation of torsemide ensures 100% bioavailability. It demonstrates a high volume of distribution and is extensively bound to plasma proteins. The compound is metabolized hepatically and excreted via renal and biliary routes, supporting its utility in patients with varying levels of renal function.
Comparative Efficacy vs. Oral Form and Other Loop Diuretics
Compared to oral torsemide, the injectable form guarantees rapid therapeutic effects. When evaluated against furosemide, torsemide exhibits a more predictable pharmacologic profile and longer duration of action, making it a favorable choice in refractory cases.
Approved Medical Uses of Torsemide Injection
Management of Edema Associated with Congestive Heart Failure
Torsemide Injection is routinely indicated to manage fluid retention in congestive heart failure. By reducing preload and alleviating pulmonary congestion, it enhances symptomatic relief and improves hemodynamics.
Treatment of Edema Due to Renal Dysfunction
In patients with impaired renal function, torsemide helps to mobilize retained fluid. Its efficacy is preserved in moderate renal insufficiency, offering reliable diuresis where thiazide diuretics are ineffective.
Edema from Hepatic Cirrhosis and Ascites Management
Torsemide Injection plays an adjunctive role in cirrhotic patients with refractory ascites. It helps reduce portal hypertension and relieves abdominal distension by promoting fluid mobilization.
Acute Management of Hypertension When Oral Therapy is Not Feasible
In hypertensive emergencies or perioperative blood pressure control, IV torsemide provides a rapid antihypertensive effect. It is particularly useful in patients unable to swallow or those with gastrointestinal limitations.
Off-Label and Investigational Uses
Adjunctive Treatment in Acute Pulmonary Edema
Torsemide Injection is often used off-label in acute pulmonary edema to relieve dyspnea by reducing pulmonary capillary wedge pressure and left ventricular filling pressures.
Use in Refractory Edema in Nephrotic Syndrome
When first-line diuretics fail to produce adequate response in nephrotic syndrome, torsemide may be introduced alone or in combination with albumin to enhance diuretic efficacy.
High-Dose Torsemide Injection in Diuretic-Resistant Cases
In cases of diuretic resistance, higher IV doses of torsemide have shown increased natriuretic response, especially when delivered via continuous infusion strategies.
Potential Use in Hyponatremia and SIADH (Syndrome of Inappropriate Antidiuretic Hormone)
Torsemide has been explored in the management of euvolemic hyponatremia due to SIADH. By promoting aquaresis while conserving sodium, it may offer a novel approach in challenging cases.
Dosage and Administration Guidelines
Recommended IV Dosage in Different Indications
- Congestive heart failure: Initial dose of 10–20 mg IV - Hepatic cirrhosis: Start with 5–10 mg IV daily - Renal insufficiency: Titrate based on urine output and creatinine
Stepwise Dosing Strategy in Diuretic Resistance
For diuretic resistance, doses may be doubled every 2–4 hours under close monitoring. Combination therapy with thiazide diuretics may enhance efficacy.
Rate of Administration and IV Push vs. Infusion
Torsemide can be administered via slow IV push over 2 minutes or as a continuous infusion. Continuous infusion is often favored in patients with limited volume tolerance.
Dose Adjustment in Renal or Hepatic Impairment
- In renal impairment: Higher doses may be needed, but with electrolyte monitoring. - In hepatic dysfunction: Dose conservatively to avoid encephalopathy.
Composition and Formulation Details
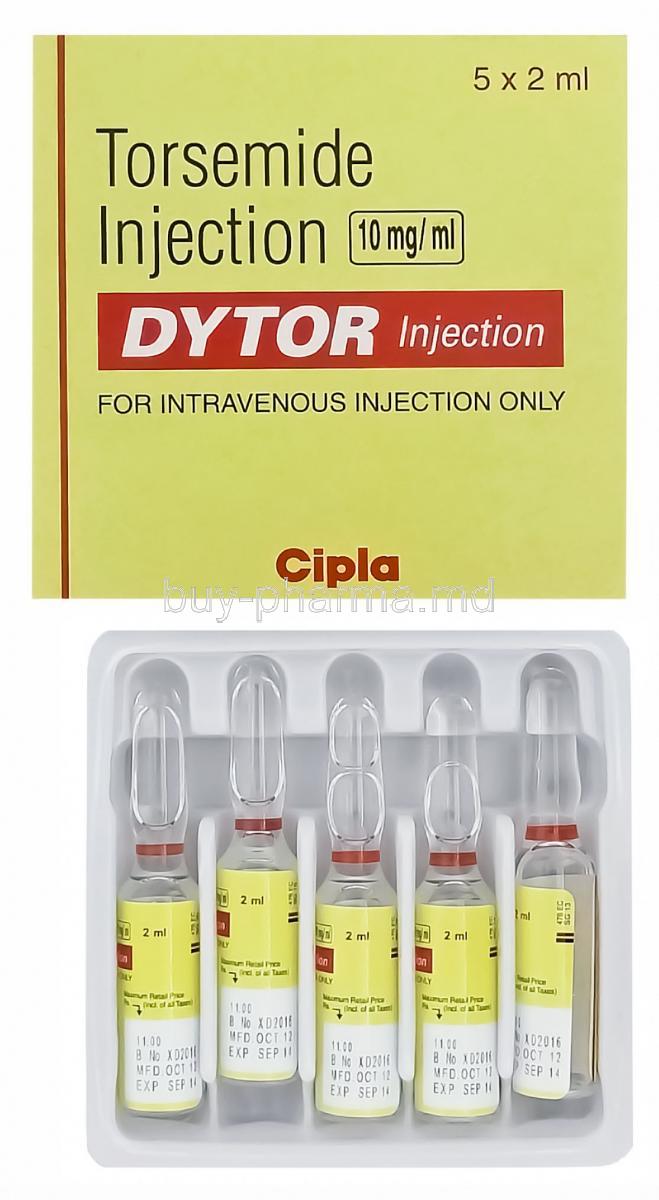
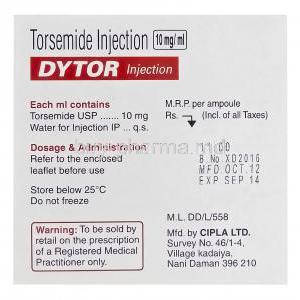
Active Ingredient: Torsemide Concentration per mL
Each mL of solution contains 10 mg of torsemide as the active component.
Inactive Ingredients and Solvent Information
Formulated with sodium hydroxide, sodium chloride, and water for injection. pH is adjusted for intravenous compatibility.
Available Packaging: Vial Sizes and Ampoules
Torsemide Injection is available in 2 mL, 5 mL, and 10 mL vials or ampoules. Single-use and preservative-free formats are standard for safety.
Storage and Stability Instructions
Ideal Storage Temperature and Conditions
Store between 20°C to 25°C (68°F to 77°F). Avoid freezing and protect from direct sunlight.
Light and Heat Sensitivity
Torsemide is light-sensitive and should be stored in its original packaging. Prolonged exposure to elevated temperatures may degrade the active compound.
Stability After Opening or Dilution
Once opened, the solution should be used immediately. If diluted in compatible IV fluids, the solution remains stable for up to 24 hours at room temperature.
Expiry and Handling of Unused Portions
Do not use if particulate matter or discoloration is observed. Discard unused portions responsibly following biohazard protocols.
Common and Serious Side Effects of Torsemide Injection
Frequently Reported Adverse Effects: Dizziness, Dehydration, Hypokalemia
Patients receiving Torsemide Injection may experience common adverse reactions related to its potent diuretic effect. Frequently reported side effects include:
- Dizziness: Often a consequence of rapid fluid loss and transient hypotension.
- Dehydration: Characterized by dry mouth, fatigue, and reduced skin turgor due to excessive diuresis.
- Hypokalemia: A notable risk, especially with prolonged use or high doses, leading to muscle cramps, arrhythmias, or fatigue.
These effects are generally manageable with dose adjustments or supplemental therapy.
Serious Adverse Events: Electrolyte Imbalance, Ototoxicity, Hypotension
Though uncommon, Torsemide Injection may cause severe reactions that require immediate clinical attention:
- Electrolyte Imbalance: Significant losses of sodium, potassium, calcium, and magnesium may lead to neuromuscular or cardiac complications.
- Ototoxicity: Hearing disturbances, including tinnitus or hearing loss, have been reported, particularly with high doses or rapid IV infusion.
- Severe Hypotension: Sudden drops in blood pressure can cause syncope or organ hypoperfusion, especially in elderly or volume-depleted patients.
Monitoring Parameters for Adverse Reactions
Continuous monitoring enhances patient safety during Torsemide therapy:
- Serum electrolytes (K⁺, Na⁺, Mg²⁺, Ca²⁺)
- Renal function tests (creatinine, BUN)
- Blood pressure and hydration status
- Auditory function in long-term or high-dose therapy
Drug Interactions and Risk of Combination Therapy
Interaction with Other Diuretics and Antihypertensives
Concurrent use with other diuretics can potentiate electrolyte loss. When combined with antihypertensives, there is an increased risk of symptomatic hypotension.
Effects When Combined with NSAIDs or Aminoglycosides
- NSAIDs: May attenuate the diuretic and antihypertensive effects of Torsemide by reducing renal perfusion. - Aminoglycosides: Co-administration may exacerbate nephrotoxicity and ototoxicity risks.
Potentiation of Digitalis and Lithium Toxicity
Torsemide-induced hypokalemia can increase the cardiotoxic potential of digitalis glycosides. Additionally, reduced renal clearance may elevate lithium levels, necessitating frequent monitoring.
Synergistic or Antagonistic Pharmacodynamic Effects
The combination of Torsemide with vasodilators or ACE inhibitors may produce synergistic hypotensive effects. Conversely, corticosteroids or laxatives may antagonize potassium conservation, amplifying hypokalemic risk.
Contraindications for Torsemide Injection
Hypersensitivity to Sulfonylurea-Derived Compounds
Patients with known allergies to sulfonylureas should avoid Torsemide due to structural similarities that may provoke hypersensitivity reactions.
Anuria and Advanced Renal Failure
Torsemide is ineffective in anuric states and may worsen fluid and electrolyte disturbances in advanced renal failure.
Severe Electrolyte Imbalance Unresponsive to Correction
Correcting imbalances such as hypokalemia or hyponatremia is a prerequisite before initiating therapy, as Torsemide may intensify these disturbances.
Warnings and Important Safety Considerations
Risk of Profound Diuresis and Volume Depletion
Torsemide's potent action can result in rapid volume depletion, leading to hypotension, renal dysfunction, and hypoperfusion. Careful titration is essential.
Monitoring of Electrolytes, Renal Function, and Blood Pressure
Regular assessments are required to prevent iatrogenic complications:
- Daily weight and fluid balance
- Electrolyte panels and renal biomarkers
- Blood pressure monitoring at multiple intervals
Caution in Patients with Hepatic Encephalopathy
Electrolyte disturbances, particularly hypokalemia and alkalosis, may precipitate hepatic encephalopathy in cirrhotic individuals.
Risk of Hearing Loss at High Doses or in Renal Dysfunction
Patients receiving high doses or those with impaired renal clearance are more vulnerable to auditory toxicity. Slow infusion and dose moderation are advised.
Careful Administration in Special Populations
Patients with Hepatic Cirrhosis and Risk of Hepatorenal Syndrome
Torsemide should be administered with caution in cirrhotic patients. Monitoring for renal function decline and encephalopathy is mandatory.
Use in Individuals with Diabetes Mellitus or Gout
- Diabetes: Torsemide may worsen glycemic control due to volume contraction and stress response. - Gout: By reducing uric acid excretion, it may precipitate gouty attacks.
Management in Those with Hypoproteinemia or Cardiovascular Instability
Protein binding affects torsemide distribution. In hypoalbuminemia or cardiovascular instability, therapeutic response may vary, necessitating dose adjustment.
Use in Elderly Patients
Altered Pharmacodynamics and Risk of Orthostatic Hypotension
The elderly may have reduced physiological reserves, increasing susceptibility to sudden blood pressure drops, falls, or electrolyte disturbances.
Dosage Adjustment Based on Renal Clearance
Creatinine clearance should guide dose titration. Start low and go slow is the preferred approach in geriatric patients.
Recommendations for Titration and Monitoring
Frequent follow-ups and laboratory monitoring are critical. Individualized dosing plans help mitigate adverse events in this vulnerable group.
Administration in Pregnancy and Lactation
Torsemide’s Pregnancy Risk Category and Animal Data
Torsemide falls under Pregnancy Category B in some jurisdictions. Although animal studies show minimal teratogenicity, controlled human studies are lacking.
Potential Fetal Risks Due to Fluid and Electrolyte Shifts
Diuretic-induced volume contraction may impair placental perfusion, potentially leading to fetal growth restriction or distress.
Excretion in Breast Milk and Breastfeeding Considerations
It is unknown whether torsemide is excreted in human milk. However, due to the potential for serious adverse reactions in nursing infants, discontinuation of breastfeeding or the drug may be required.
Administration to Pediatric Patients
Limited Clinical Data and Use Only When Clearly Indicated
There is a scarcity of clinical data on pediatric safety and efficacy. Use is generally restricted to hospital settings under specialist care.
Weight-Based Dosing Recommendations
Dosing should follow pediatric-specific protocols, typically in mg/kg, with adjustments based on response and renal function.
Monitoring Requirements in Neonates and Infants
Close monitoring of hydration status, serum electrolytes, and urine output is mandatory in neonates due to immature renal handling of solutes.
Overdose and Emergency Management
Symptoms of Acute Overdose: Hypovolemia, Electrolyte Imbalance, Hypotension
Signs of overdose may include:
- Profound hypotension
- Severe dehydration and electrolyte loss
- Renal dysfunction or acute kidney injury
Recommended Emergency Interventions and Supportive Care
- Discontinue torsemide immediately. - Initiate intravenous volume replacement with isotonic fluids. - Correct electrolyte imbalances with appropriate supplements.
Role of Dialysis and Hemodynamic Monitoring
Hemodialysis may aid in fluid management but is not highly effective in removing torsemide. Continuous hemodynamic monitoring is essential during recovery.
Safe Handling and Precautionary Measures
Aseptic Technique for IV Administration
All injections must be prepared and administered using strict aseptic technique to prevent contamination and infection.
Disposal of Sharps and Leftover Medication
Used vials, ampoules, and needles should be disposed of in puncture-resistant containers. Residual drug should be discarded per institutional protocols.
Occupational Exposure Risks and Protective Measures for Healthcare Staff
Personnel handling the injection should wear gloves and protective clothing. Any accidental exposure, particularly splashes to eyes or skin, should be addressed with immediate irrigation and medical evaluation.
Torsemide Injection FAQ
- What is the use of torsemide injection?
- Does torsemide have IV?
- What is the drug torsemide used for?
- How to give IV torsemide?
- Is torsemide safe for kidneys?
- What is the best time of day to take torsemide?
- How long is torsemide effective?
- Can torsemide be given IV push?
- What are the side effects of torsemide injections?
- What is the side effect of torsemide?
- Can torsemide increase creatinine?
- Do you need to take potassium with torsemide?
- Can you take torsemide without food?
- What to avoid when taking torsemide?
- What should I monitor when taking torsemide?
- How many torsemide per day?
- What is a substitute for torsemide?
- Is torsemide good for kidneys?
- Can I take torsemide at night?
- Is torsemide a strong diuretic?
- Can torsemide lower platelet count?
- Is torsemide safer than furosemide?
- What are the serious side effects of torsemide?
- How long can you take torsemide?
What is the use of torsemide injection?
Torsemide is commonly prescribed to manage edema, the accumulation of fluid in body tissues due to conditions like heart issues or kidney and liver diseases.
Does torsemide have IV?
Torsemide can also be administered via injection for the onset of diuretic action or in situations where oral medication is not feasible.
What is the drug torsemide used for?
Torsemide is prescribed to assist with managing retention (edema), which may arise from heart failure, as well as liver or kidney disease.
How to give IV torsemide?
Administer the medication rapidly over 2 minutes. Deliver it steadily through an infusion.
Is torsemide safe for kidneys?
As individuals get older, they may experience poor blood flow to organs like the kidneys.
What is the best time of day to take torsemide?
It's recommended to take Torsemide 4 hours before going to bed.
How long is torsemide effective?
6 to 8 hours
Can torsemide be given IV push?
Yes
What are the side effects of torsemide injections?
- frequent urination
- headache
- cough
- sore throat
- hearingloss
- ringing in your ears
- upset stomach
- constipation
What is the side effect of torsemide?
- frequent urination
- headache
- cough
- sore throat
- hearingloss
- ringing in your ears
- upset stomach
- constipation
Can torsemide increase creatinine?
Yes
Do you need to take potassium with torsemide?
Your healthcare provider may suggest that you take this medication alongside potassium supplements to help regulate your electrolyte levels.
Can you take torsemide without food?
Yes
What to avoid when taking torsemide?
Torsemide and alcohol (ethanol), when taken together, may work together to lower your blood pressure effectively. They could result in symptoms such as headaches, dizziness, lack of balance, fainting, and variations in heart rate or pulse.
What should I monitor when taking torsemide?
Torsemide might lead to feelings of dizziness and faintness when you stand up quickly after lying down.
How many torsemide per day?
The amount of torsemide you take varies depending on the health issue you're addressing as an adult. The typical initial dose is between 5 mg and 20 mg taken daily. The highest dose may range from 40 mg to 200 mg per day, depending on the condition being treated.
What is a substitute for torsemide?
Furosemide or Carvedilol
Is torsemide good for kidneys?
Torsemide is a drug prescribed to decrease the buildup of fluids and swelling (edema) commonly linked to heart failure and conditions like kidney or liver disease (cirrhosis).
Can I take torsemide at night?
Try not to take this medicine at bedtime as it might cause you to wake up during the night to use the bathroom.
Is torsemide a strong diuretic?
Torsemide's strong water-reducing power can result in body fluid loss, which may lead to dehydration and electrolyte depletion.
Can torsemide lower platelet count?
Yes
Is torsemide safer than furosemide?
Both torsemide and furosemide function in a manner that results in them sharing a safety profile.
What are the serious side effects of torsemide?
- Signs of dehydration and electrolyte imbalance include having a dry mouth and feeling thirsty or nauseous.
- Vomiting or weakness, leading to tiredness and drowsiness
- Restlessness or confusion
- Muscle weakness or pain accompanied by cramps and a fast heartbeat.
How long can you take torsemide?
To effectively reduce your blood pressure and maintain it at a level, be sure to follow the recommended directions.