Introduction
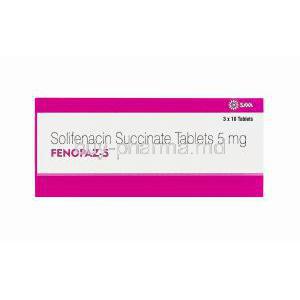
Overview of Fenopaz (brand name for Solifenacin)
Fenopaz, known generically as Solifenacin, is a pharmacological agent primarily prescribed for the management of bladder control disorders. It belongs to a category of medicines that diminish involuntary contractions of the bladder, offering relief to individuals burdened by persistent urinary urgency and frequency. By enhancing bladder storage capacity, Fenopaz significantly improves quality of life for patients suffering from overactive bladder syndromes.
Therapeutic classification: antimuscarinic agent for bladder disorders
This medication is classified as an antimuscarinic agent. It acts selectively on muscarinic receptors located in the bladder, thereby moderating neural signals that cause inappropriate contractions. Its therapeutic profile is distinct from diuretics or alpha-blockers, focusing solely on modulating smooth muscle activity within the urinary system.
Historical background and clinical approval timeline
Solifenacin was introduced after extensive clinical trials demonstrated its efficacy and safety in treating overactive bladder (OAB). Approved by regulatory authorities in the early 2000s, it quickly gained recognition as a first-line treatment option for OAB. Its approval marked a pivotal moment, as it provided a well-tolerated alternative to older anticholinergic drugs that carried higher rates of central nervous system side effects.
Comparison with other overactive bladder treatments
Compared to other therapeutic agents such as tolterodine or oxybutynin, Fenopaz demonstrates improved receptor selectivity and fewer cognitive adverse events. It also offers the advantage of once-daily dosing, which contributes to higher patient adherence. While beta-3 adrenergic agonists like mirabegron are also prescribed, solifenacin remains widely utilized due to its established safety record and effectiveness in long-term use.
Composition and Formulation
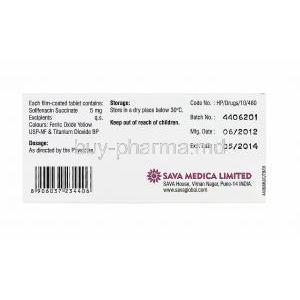
Active ingredient: Solifenacin succinate
Fenopaz contains solifenacin succinate as its active pharmaceutical ingredient. This salt form enhances stability and bioavailability, ensuring consistent therapeutic effects.
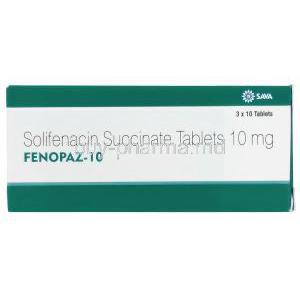
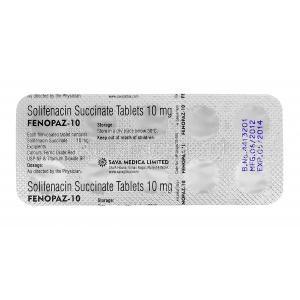
Available strengths and dosage forms
Fenopaz is available in tablet form, typically supplied in 5 mg and 10 mg strengths. Film-coated tablets improve patient compliance by easing ingestion and reducing irritation during administration.
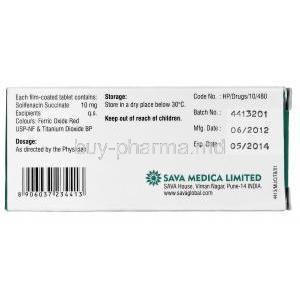
Inactive ingredients and excipients
Excipients include lactose monohydrate, maize starch, and hypromellose. These components stabilize the formulation, assist in tablet disintegration, and enhance absorption.
How Fenopaz (Solifenacin) Works
Mechanism of action as a selective muscarinic receptor antagonist
Fenopaz acts by selectively blocking M3 muscarinic receptors located on bladder smooth muscle. By antagonizing these receptors, it diminishes cholinergic stimulation responsible for involuntary detrusor contractions.
Effects on bladder smooth muscle contraction and storage function
Through receptor antagonism, Fenopaz prolongs bladder filling time, increases bladder capacity, and delays the urge to urinate. This translates to fewer episodes of urgency and reduced frequency of incontinence.
Pharmacokinetics: absorption, distribution, metabolism, and elimination
- Absorption: Rapidly absorbed with peak plasma concentrations within 3–8 hours.
- Distribution: Extensive tissue distribution with high protein binding.
- Metabolism: Primarily metabolized by hepatic CYP3A4 enzymes.
- Elimination: Excreted via urine and feces, with a half-life of approximately 45–68 hours, enabling once-daily dosing.
Uses of Fenopaz (Approved Indications)
Treatment of overactive bladder with symptoms of urgency
Fenopaz is clinically indicated for the management of overactive bladder, particularly in patients experiencing sudden, uncontrollable urges to urinate.
Management of increased daytime urinary frequency
The drug helps reduce the number of daytime urination episodes, thereby restoring normal voiding patterns and minimizing disruptions in daily life.
Control of urge urinary incontinence
By reducing detrusor overactivity, Fenopaz provides reliable control over involuntary urine leakage, improving patient dignity and comfort.
Off-Label Uses of Solifenacin
Potential role in neurogenic detrusor overactivity (NDO)
In patients with neurological disorders such as spinal cord injury, solifenacin may help reduce uncontrolled detrusor contractions, although this remains off-label.
Use in pediatric patients with refractory bladder dysfunction
Investigational studies suggest potential benefit in children with severe bladder dysfunction unresponsive to other therapies. However, its safety profile in this group is still under evaluation.
Adjunct therapy in interstitial cystitis/painful bladder syndrome
Though not officially approved, some clinicians employ solifenacin as part of a multidrug regimen to reduce urgency and bladder discomfort in patients with chronic pelvic pain syndromes.
Role in treating urinary symptoms in multiple sclerosis and Parkinson’s disease patients
Patients with neurodegenerative disorders often experience bladder dysfunction. Fenopaz has shown promise in mitigating these symptoms when conventional treatments fall short.
Dosage and Administration
Standard recommended dosages for adults
The typical starting dose is 5 mg once daily, which may be increased to 10 mg daily depending on patient response and tolerability.
Initial dose vs. maintenance dose considerations
Clinicians often initiate therapy at 5 mg to assess tolerance before escalating to the full 10 mg dose for sustained symptom control.
Adjustment guidelines based on clinical response
Dose modifications are guided by the severity of symptoms, patient comorbidities, and side effect occurrence. In patients with renal or hepatic impairment, lower doses may be necessary.
Administration instructions
- May be taken with or without food.
- Should be swallowed whole with water, not chewed or crushed.
- Best taken at the same time daily to maintain consistent plasma levels.
Special Administration Guidelines
Administration to elderly patients
Elderly patients may be more susceptible to anticholinergic side effects such as constipation and cognitive impairment. Careful monitoring and possible dose adjustments are recommended.
Administration to pregnant women
There is limited clinical data regarding solifenacin use in pregnancy. It should only be used if the potential benefit outweighs the possible risk to the fetus.
Administration to nursing mothers
Because solifenacin may be excreted in breast milk, caution is advised. Alternative therapies may be considered to avoid infant exposure.
Administration to children
The safety and efficacy of solifenacin in children have not been firmly established. Use is restricted to investigational or specialist-guided contexts.
Side Effects of Fenopaz
Common Side Effects
- Dry mouth and constipation
- Blurred vision and drowsiness
- Urinary tract infections and dyspepsia
- Headache and fatigue
Serious Adverse Reactions
- Urinary retention, particularly in patients with bladder outlet obstruction
- Severe constipation that may progress to bowel obstruction
- QT prolongation and potential cardiac arrhythmias
- Hypersensitivity reactions including rash and anaphylaxis
Drug Interactions
Interactions with CYP3A4 inhibitors
Potent CYP3A4 inhibitors such as ketoconazole and ritonavir may elevate plasma solifenacin concentrations, leading to enhanced adverse effects.
Interactions with CYP3A4 inducers
Drugs like rifampicin and carbamazepine accelerate metabolism of solifenacin, reducing its therapeutic efficacy.
Concurrent use with other anticholinergics
Combining Fenopaz with other anticholinergics can amplify side effects such as dry mouth, blurred vision, and constipation.
Interaction with drugs affecting cardiac rhythm
Caution is warranted when prescribing alongside medications that prolong the QT interval, as this may increase arrhythmic risk.
Warnings and Important Precautions
Risk of urinary retention in patients with bladder outlet obstruction
Fenopaz (solifenacin) may exacerbate urinary retention in individuals with bladder outlet obstruction. Patients should be closely monitored for worsening voiding difficulties, and therapy must be discontinued if retention develops. The risk is heightened in men with enlarged prostate glands and in those with underlying urological abnormalities.
Caution in patients with gastrointestinal obstructive disorders
Due to its antimuscarinic properties, Fenopaz should be used with caution in patients with gastrointestinal obstructive disorders. These individuals may experience aggravated motility disturbances, increasing the likelihood of ileus, constipation, or abdominal pain.
Monitoring for QT prolongation in cardiac patients
QT interval prolongation has been reported with solifenacin, particularly at higher doses or in combination with other QT-prolonging agents. Patients with preexisting heart disease, electrolyte disturbances, or those on antiarrhythmic therapy should undergo careful electrocardiographic monitoring.
Avoidance in uncontrolled narrow-angle glaucoma
Fenopaz is contraindicated in patients with uncontrolled narrow-angle glaucoma. Its anticholinergic activity may further increase intraocular pressure, precipitating acute glaucomatous attacks and vision loss.
Contraindications
Hypersensitivity to solifenacin or excipients
Patients with known hypersensitivity to solifenacin or any of the tablet’s inactive ingredients should not take Fenopaz. Hypersensitivity reactions may manifest as rash, pruritus, or anaphylaxis.
Patients with urinary retention
Solifenacin is strictly contraindicated in patients with existing urinary retention. The drug’s mechanism may worsen retention, leading to acute urological emergencies.
Severe gastrointestinal conditions (e.g., toxic megacolon)
Individuals with severe gastrointestinal conditions, particularly toxic megacolon, are at risk of worsened outcomes with solifenacin use. Suppression of bowel motility may be life-threatening in such conditions.
Myasthenia gravis
Patients diagnosed with myasthenia gravis must not be prescribed Fenopaz. Anticholinergic medications may exacerbate muscular weakness, potentially impairing respiratory function.
Careful Administration Considerations
Patients with hepatic impairment: dose limitations and monitoring
For patients with moderate hepatic impairment, dosage should not exceed 5 mg daily. Severe hepatic impairment precludes safe administration, and close monitoring of liver function is essential during therapy.
Patients with renal impairment: dose adjustment recommendations
In moderate to severe renal impairment, the maximum recommended dose is reduced to 5 mg daily. Renal insufficiency may prolong drug clearance, thereby intensifying side effects.
Patients with autonomic neuropathy
Autonomic neuropathy, often associated with diabetes or neurodegenerative disorders, may amplify the anticholinergic effects of Fenopaz. Clinical vigilance is required to prevent adverse outcomes such as severe constipation or urinary difficulties.
Polypharmacy risks in elderly and frail patients
Elderly or frail patients often take multiple medications, increasing the risk of drug-drug interactions and cumulative anticholinergic burden. Careful medication review and regular reassessment of therapy necessity are strongly advised.
Overdosage
Symptoms of overdose: confusion, hallucinations, severe anticholinergic effects
Overdosage may present with pronounced anticholinergic toxicity, including confusion, agitation, visual hallucinations, blurred vision, severe dry mouth, tachycardia, and urinary retention.
Emergency management strategies
Initial treatment should focus on stabilization of vital functions, airway management, and cardiac monitoring. Prompt recognition of overdose symptoms enhances the likelihood of full recovery.
Role of supportive therapy and gastric lavage
Supportive measures, including intravenous hydration and correction of electrolyte imbalance, are critical. Gastric lavage may be considered if ingestion is recent and the patient presents within one hour of overdose.
Antidote considerations and hospital observation
No specific antidote exists for solifenacin toxicity. Patients should be admitted for hospital observation, particularly when severe symptoms manifest, to mitigate the risks of arrhythmia and central nervous system complications.
Storage and Handling Precautions
Recommended storage conditions: temperature, light, and moisture protection
Fenopaz should be stored at controlled room temperature, away from excessive heat and direct sunlight. Tablets must be kept in their original packaging to protect against moisture degradation.
Shelf life and stability of tablets
Each blister pack includes a manufacturer’s expiration date. Use beyond this date is discouraged as chemical stability and therapeutic potency cannot be guaranteed.
Handling instructions for healthcare providers and caregivers
Tablets should not be crushed or broken, as this may alter drug delivery. Caregivers must ensure patients adhere strictly to prescribed dosages.
Safe disposal of unused or expired medication
Unused or expired medication should be disposed of in accordance with local pharmaceutical waste guidelines. Flushing into water systems is discouraged due to potential environmental hazards.