Introduction to Tasigna (Nilotinib)
Overview of Tasigna and its Role in Cancer Therapy
Tasigna, also known by its generic name nilotinib, is a targeted therapy designed to inhibit abnormal cell signaling in certain cancers. It is primarily prescribed for chronic myeloid leukemia (CML), where it helps restore hematologic balance by halting malignant proliferation. By focusing on precise molecular pathways, Tasigna has transformed the management of CML, offering patients improved outcomes and quality of life.
History of Approval and Clinical Significance
Nilotinib was developed as a second-generation tyrosine kinase inhibitor (TKI), gaining approval by the U.S. Food and Drug Administration (FDA) in 2007. Its clinical significance lies in its ability to provide effective treatment for patients resistant or intolerant to earlier therapies such as imatinib. Over time, Tasigna has become an indispensable therapeutic option, with widespread acceptance in oncology practice worldwide.
Distinction Between Tasigna and Other Tyrosine Kinase Inhibitors (TKIs)
Unlike first-generation TKIs, Tasigna demonstrates a more potent and selective inhibition of the BCR-ABL oncoprotein. Its refined molecular design allows it to combat resistant mutations, achieving deeper and more durable responses. This distinction makes Tasigna not just an alternative but, in many cases, a superior choice for patients requiring sustained disease control.
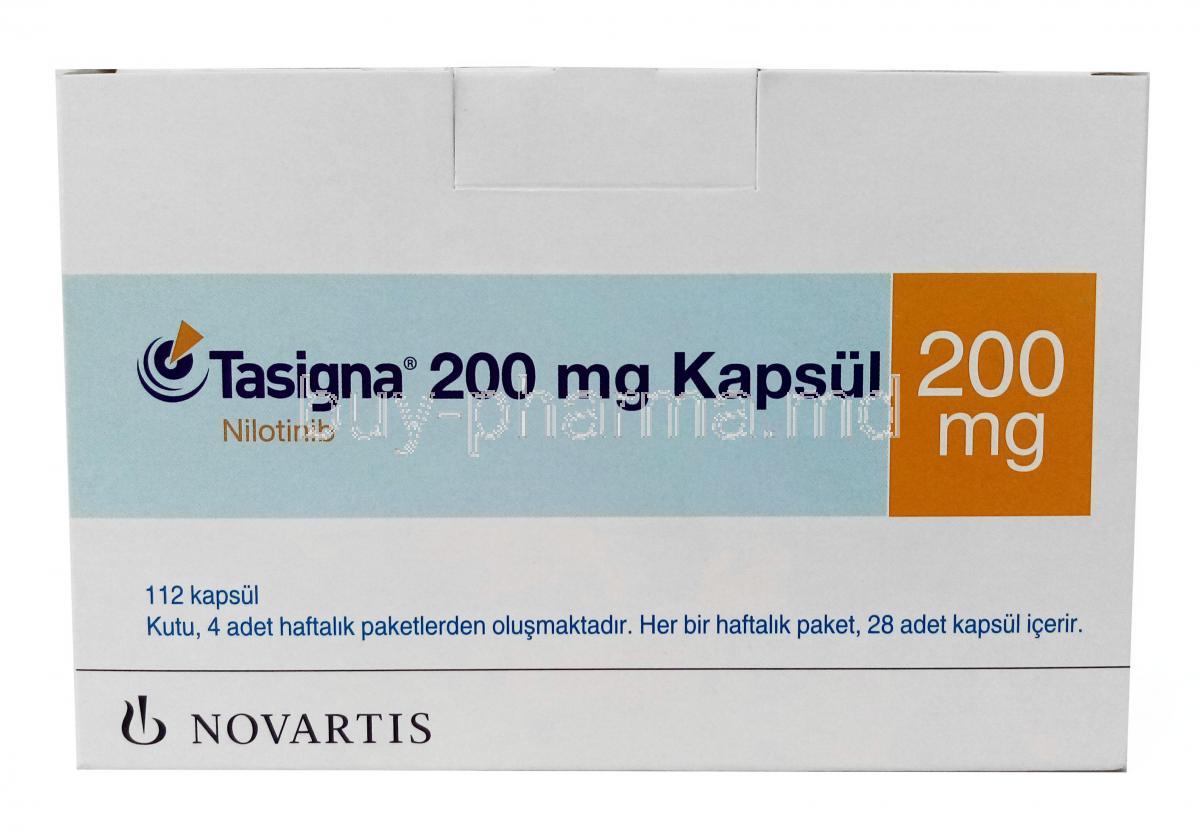
Composition and Active Ingredients
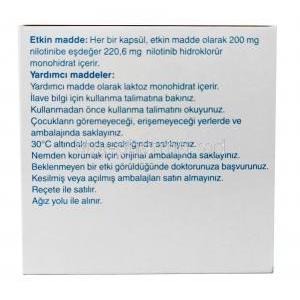
Active Ingredient: Nilotinib Hydrochloride Monohydrate
The therapeutic core of Tasigna is nilotinib hydrochloride monohydrate, a compound meticulously engineered to block the activity of abnormal tyrosine kinases driving CML pathology.
Inactive Ingredients and Formulation Specifics
Tasigna capsules contain pharmaceutical excipients that ensure drug stability and absorption. These include lactose monohydrate, crospovidone, magnesium stearate, and other agents essential for capsule integrity and bioavailability.
Available Dosage Strengths and Pharmaceutical Forms
Tasigna is available in capsule form, typically in 150 mg and 200 mg strengths, enabling flexibility in dosing regimens tailored to individual patient needs.
How Tasigna Works: Mechanism of Action
Targeting BCR-ABL Tyrosine Kinase Activity
Tasigna exerts its antineoplastic effect by binding to the ATP-binding site of the BCR-ABL kinase. This action prevents the enzyme from activating downstream signaling cascades that fuel malignant cell growth.
Inhibition of Abnormal Signaling Pathways in CML
By suppressing aberrant signaling, Tasigna halts the uncontrolled proliferation of leukemic cells. This translates into reduced tumor burden and restoration of normal hematopoietic function.
Impact on Leukemic Cell Proliferation and Survival
- Induces apoptosis in malignant cells
- Reduces leukemic stem cell survival
- Inhibits disease progression at the molecular level
Differences Compared to Imatinib and Other TKIs
Nilotinib is approximately 20–30 times more potent than imatinib in inhibiting BCR-ABL activity. It is also effective against certain imatinib-resistant mutations, offering broader therapeutic coverage.
Approved Medical Uses of Tasigna
Treatment of Philadelphia Chromosome-Positive (Ph+) Chronic Myeloid Leukemia (CML) in Chronic Phase
Tasigna is specifically indicated for adult patients with Ph+ CML in the chronic phase, providing a targeted therapeutic avenue for this hematologic malignancy.
Indications for Newly Diagnosed Patients
For patients newly diagnosed with CML, Tasigna offers the possibility of achieving early molecular responses, which correlate with long-term survival benefits.
Use in Patients Resistant or Intolerant to Prior Therapies Including Imatinib
Tasigna is a crucial option for patients who fail to respond adequately to imatinib, ensuring continuity of effective treatment while minimizing disease progression risks.
Off-Label and Investigational Uses of Nilotinib
Research in Acute Lymphoblastic Leukemia (ALL)
Studies are evaluating nilotinib’s efficacy in Ph+ ALL, where BCR-ABL abnormalities also play a pathogenic role.
Potential Application in Systemic Mastocytosis
Nilotinib is being investigated for its role in suppressing abnormal mast cell proliferation in systemic mastocytosis, a rare hematologic condition.
Studies in Gastrointestinal Stromal Tumors (GISTs)
Research continues on nilotinib’s ability to inhibit c-KIT and PDGF receptors, pathways relevant in GISTs.
Emerging Evidence in Neurodegenerative Conditions Such as Parkinson’s Disease and Alzheimer’s Disease
Experimental findings suggest nilotinib may promote clearance of neurotoxic proteins, sparking interest in its potential for neurological disorders.
Role in Precision Oncology and Targeted Therapies
Nilotinib exemplifies the movement toward precision medicine, where therapy is tailored based on specific genetic and molecular abnormalities.
Dosage and Administration Guidelines
Standard Dosing Regimens for Adults with CML
The typical recommended dose is 300 mg taken orally twice daily. Consistent dosing is essential to maintain steady plasma concentrations.
Dose Adjustment Based on Response and Tolerance
Dosage may be modified in the event of severe side effects, suboptimal response, or drug interactions. Adjustments are guided by regular clinical and laboratory evaluations.
Instructions Regarding Food Intake and Timing of Administration
Tasigna must be taken on an empty stomach. Food increases systemic exposure and raises the risk of QT prolongation. Patients should avoid eating for two hours before and one hour after each dose.
Monitoring Requirements During Therapy
Frequent monitoring of complete blood counts, liver function, and ECG is required to ensure safety and efficacy during treatment.
Administration Considerations in Hepatic or Renal Impairment
Patients with hepatic dysfunction require careful dose management, while renal impairment necessitates close observation though no specific dose reduction may be immediately required.
Common Side Effects of Tasigna
Gastrointestinal Disturbances: Nausea, Diarrhea, Constipation
Digestive tract symptoms are among the most frequently reported, though often manageable with supportive care.
Fatigue, Headache, Rash, and Pruritus
These non-specific adverse reactions are typically mild to moderate in severity but may impact quality of life if persistent.
Musculoskeletal Pain and Arthralgia
Patients may experience joint discomfort and muscle aches, often alleviated with symptomatic management.
Laboratory Abnormalities: Elevated Bilirubin, Lipase, and Liver Enzymes
Regular biochemical monitoring is essential to detect subclinical changes in hepatic and pancreatic function.
Serious and Rare Side Effects
QT Prolongation and Arrhythmia Risk
Tasigna carries a known risk of prolonging the QT interval, necessitating careful cardiac monitoring. Life-threatening arrhythmias may occur in susceptible individuals.
Myelosuppression: Neutropenia, Anemia, Thrombocytopenia
Bone marrow suppression can lead to cytopenias, requiring dose modification or temporary discontinuation.
Pancreatitis and Hepatotoxicity
Rare but severe, inflammation of the pancreas and liver toxicity may demand immediate intervention.
Metabolic Effects: Hyperglycemia, Lipid Abnormalities
Tasigna can alter glucose and lipid metabolism, potentially predisposing patients to cardiovascular complications.
Vascular Occlusive Events
Cases of arterial and venous occlusive events, including peripheral arterial disease and ischemic stroke, have been documented, necessitating vigilant risk assessment and monitoring.
Drug Interactions
Interaction with CYP3A4 Inhibitors and Inducers
Tasigna is primarily metabolized by the cytochrome P450 3A4 (CYP3A4) enzyme. Strong CYP3A4 inhibitors, such as ketoconazole, clarithromycin, and ritonavir, can significantly elevate plasma concentrations of nilotinib, increasing the risk of toxicity. Conversely, CYP3A4 inducers like rifampin, carbamazepine, or phenytoin reduce drug exposure, potentially leading to therapeutic failure. Physicians must avoid co-administration or adjust treatment plans accordingly.
Effects of Proton Pump Inhibitors, H2 Blockers, and Antacids
Nilotinib absorption is influenced by gastric pH. Proton pump inhibitors (PPIs) may reduce absorption, leading to subtherapeutic exposure. H2 blockers and antacids should be administered at staggered intervals to minimize interaction, with careful adherence to recommended timing protocols to ensure efficacy.
Interactions with Anticoagulants, Antiarrhythmics, and Other Cancer Therapies
Concurrent use of anticoagulants such as warfarin or direct oral anticoagulants necessitates close monitoring due to altered metabolism and increased bleeding risk. Antiarrhythmic medications including amiodarone or quinidine may compound the risk of QT prolongation. Additionally, the combination with other oncologic therapies may amplify hematologic and hepatic toxicities, requiring multidisciplinary oversight.
Grapefruit Juice and Dietary Considerations
Grapefruit juice acts as a potent CYP3A4 inhibitor, markedly increasing nilotinib plasma levels. Patients must avoid grapefruit and related citrus products. Furthermore, strict adherence to fasting conditions around each dose is essential, as food intake enhances absorption and increases the likelihood of adverse cardiac events.
Warnings and Important Precautions
Black Box Warning: QT Prolongation and Sudden Death Risk
Tasigna carries a boxed warning due to the risk of QT interval prolongation and sudden cardiac death. Clinicians must evaluate baseline cardiac status prior to initiation and throughout therapy.
Monitoring of EKG and Electrolytes
Regular electrocardiograms (EKG) are recommended at baseline, after dose adjustments, and periodically during treatment. Electrolyte levels, especially potassium and magnesium, must be corrected to reduce arrhythmic risk.
Risks of Sudden Discontinuation
Abrupt cessation may result in rapid disease progression. Any decision to stop treatment should be undertaken under medical supervision with careful transition planning.
Patient Education on Adherence and Safety Measures
Patients should be counseled on strict dosing schedules, the importance of fasting before and after each dose, and recognition of potential cardiac symptoms. Education empowers patients to manage therapy safely and effectively.
Contraindications
Known Hypersensitivity to Nilotinib or Any Excipient
Individuals with a history of hypersensitivity reactions to nilotinib or capsule components should not receive Tasigna.
Use in Patients with Significant Baseline QT Prolongation
Tasigna is contraindicated in patients with congenital long QT syndrome or clinically significant baseline QT prolongation due to the heightened risk of arrhythmia.
Severe Hepatic Impairment Where Risk Outweighs Benefits
In patients with advanced hepatic dysfunction, nilotinib metabolism may be severely impaired, leading to elevated systemic exposure and toxicity. Use is generally not recommended in this population.
Careful Administration in Special Populations
Elderly Patients
Older adults may experience altered pharmacokinetics due to age-related physiological changes. The risk of comorbidities and polypharmacy further complicates therapy, necessitating individualized dose adjustments and closer monitoring for cardiovascular and metabolic complications.
Pregnant Women and Nursing Mothers
Nilotinib is categorized as potentially teratogenic, with data suggesting risks of fetal harm and placental toxicity. It is contraindicated during pregnancy unless the potential benefit outweighs the risk. The drug is excreted in breast milk; therefore, breastfeeding is strongly discouraged during treatment to prevent neonatal exposure.
Pediatric and Adolescent Use
Tasigna is approved for use in pediatric CML in certain regions. While studies demonstrate efficacy, long-term safety requires careful surveillance. Monitoring growth, development, and endocrine function is vital for younger patients undergoing extended therapy.
Overdosage and Emergency Management
Symptoms of Overdose and Potential Complications
Overdose may manifest as severe myelosuppression, hepatotoxicity, or cardiac arrhythmias including life-threatening QT prolongation. Gastrointestinal distress such as nausea and vomiting may also occur.
Immediate Supportive Care and Monitoring Protocols
Supportive measures should be instituted promptly, including continuous cardiac monitoring, correction of electrolyte disturbances, and symptomatic management. Hematologic and hepatic parameters require urgent evaluation.
Lack of Specific Antidote and Role of Gastric Lavage/Charcoal
No specific antidote exists for nilotinib overdose. Gastric lavage or activated charcoal may be considered if ingestion is recent. The mainstay of management remains supportive care and vigilant monitoring.
Storage and Handling Precautions
Recommended Storage Conditions for Tasigna Capsules
Capsules should be stored at controlled room temperature, protected from excessive heat, moisture, and direct sunlight to maintain drug integrity.
Stability and Shelf Life Information
Tasigna maintains stability for the duration of its manufacturer-defined shelf life when stored under recommended conditions. Expired products should not be used due to potential loss of efficacy and safety.
Safe Handling Guidelines for Healthcare Professionals and Caregivers
Healthcare providers should handle Tasigna capsules with care, minimizing unnecessary exposure. Capsules should not be opened or crushed, as this may alter bioavailability and increase occupational exposure risks.
Disposal Instructions for Unused or Expired Medication
Unused or expired Tasigna must be disposed of in compliance with local pharmaceutical waste regulations. Patients should be advised against discarding medication in household trash or wastewater systems.
Tasigna, Nilotinib FAQ
- What is the drug Tasigna used for?
- Is Tasigna considered chemotherapy?
- What to avoid while taking Tasigna?
- What happens if you stop taking Tasigna?
- Can Tasigna cause hair loss?
- Can I drink coffee after taking Tasigna?
- Is Tasigna chemo?
- What is the generic name for Tasigna?
- Does Tasigna increase blood sugar?
- What are the side effects of Tasigna nilotinib?
- What is the drug nilotinib used for?
- Is nilotinib a chemo drug?
- What is the difference between imatinib and nilotinib?
- What is the mechanism of action of nilotinib?
- What should I avoid while taking nilotinib?
- How long do you take nilotinib?
- How does nilotinib affect the heart?
- What is the success rate of nilotinib?
- Is nilotinib FDA approved?
- Does nilotinib cause memory loss?
- What happens if you stop taking nilotinib?
- What tests are needed while on nilotinib?
- What foods should be avoided with nilotinib?
- Can nilotinib cause stroke?
- How effective is nilotinib?
- Does nilotinib cause weight gain?
- Can nilotinib cause pancreatitis?
- What are the side effects of the drug nilotinib?
- When to stop nilotinib?
What is the drug Tasigna used for?
Tasigna, an agent, for myelogenous leukaemia (CML)—a blood‑cancer malignancy—is employed in individuals who have just been diagnosed or in those for whom alternative cancer drugs, such as imatinib, prove either intolerably toxic or simply ineffective.
Is Tasigna considered chemotherapy?
Yes
What to avoid while taking Tasigna?
Grapefruit
What happens if you stop taking Tasigna?
When the Tasigna regimen is halted, patients may experience a collection of aches, including musculoskeletal pain, lingering myalgia in the extremities, arthralgic joint discomfort, bone pain, and pain radiating through the spine.
Can Tasigna cause hair loss?
Yes
Can I drink coffee after taking Tasigna?
Yes
Is Tasigna chemo?
Yes
What is the generic name for Tasigna?
Nilotinib
Does Tasigna increase blood sugar?
Yes
What are the side effects of Tasigna nilotinib?
- Rash
- Relentless itching
- Queasy nausea
- Vomiting
- Diarrhea
- Constipation
What is the drug nilotinib used for?
Nilotinib is leveraged in the arsenal against a spectrum of malignancies, including pancreatic cancer, small‑cell lung cancer, liver cancer, kidney cancer, thyroid cancer, blood cancer (chronic myeloid leukaemia), gastrointestinal stromal tumour, cancers of the colon and rectum, non‑small‑cell lung cancer, soft‑tissue sarcoma, and chronic idiopathic myelofibrosis.
Is nilotinib a chemo drug?
It isn’t classified as a chemotherapy (“chemo”) treatment.
What is the difference between imatinib and nilotinib?
Nilotinib, a second‑generation tyrosine‑kinase inhibitor is thirty times more potent than imatinib.
What is the mechanism of action of nilotinib?
Nilotinib pulls its lever by acting as a Bcr‑Abl tyrosine‑kinase inhibitor then slipping into the role of a CYP2C8 inhibitor next taking on the mantle of a CYP2D6 inhibitor later flipping a switch to induce CYP2B6 then nudging CYP2C8 into induction thereafter clamping down on UGT1A1 and finally putting the brakes on the P‑glycoprotein pump.
What should I avoid while taking nilotinib?
Grapefruit
How long do you take nilotinib?
Long-term
How does nilotinib affect the heart?
Yes
What is the success rate of nilotinib?
96%
Is nilotinib FDA approved?
Yes
Does nilotinib cause memory loss?
Yes
What happens if you stop taking nilotinib?
Disease relapse
What tests are needed while on nilotinib?
- Blood tests
- Electrocardiograms (EKGs, which record the heart’s activity)
What foods should be avoided with nilotinib?
Grapefruit
Can nilotinib cause stroke?
Yes
How effective is nilotinib?
87% survival rate, 64% progression rate
Does nilotinib cause weight gain?
Rapid weight gain
Can nilotinib cause pancreatitis?
Rarely
What are the side effects of the drug nilotinib?
- Stomach pain
- Nauea
- Fever
- Sore throat
- Infection
- Edema
- Shortness of breath
When to stop nilotinib?
The protocol requires patients to have been on the medication for no more than three years.