1. Introduction to Erlocip (Erlotinib)
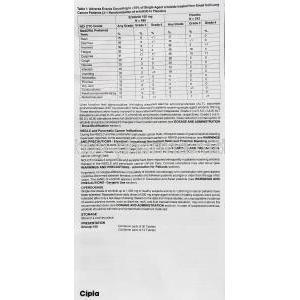
1.1 Overview of Erlocip as an Epidermal Growth Factor Receptor (EGFR) Inhibitor
Erlocip, containing the potent molecule erlotinib, functions as a selective inhibitor of the epidermal growth factor receptor (EGFR) tyrosine kinase. By targeting this receptor, the medication disrupts aberrant cellular signaling that drives malignant proliferation. Its precision-based mechanism allows it to impede tumor growth while preserving non-malignant tissues to a significant degree.
1.2 Development Background and Pharmacological Classification
Erlotinib belongs to the class of small-molecule tyrosine kinase inhibitors (TKIs). Developed through advanced molecular engineering, it was designed to intervene directly at the intracellular catalytic domain of EGFR. Over time, erlotinib has become a cornerstone therapy in precision oncology, particularly for malignancies driven by specific EGFR-activating mutations.
1.3 Key Therapeutic Roles in Oncology
The therapeutic indications for Erlocip span several high-impact oncologic conditions. Its primary benefits include:
- Targeted suppression of EGFR-driven tumors.
- Delay of disease progression in metastatic cancers.
- Improved quality of life through oral, patient-friendly therapy.
1.4 Brand Names, Generic Names, and Global Availability
Erlocip is the branded formulation of erlotinib, widely available across international oncology markets. Numerous generics exist, expanding accessibility for global cancer treatment programs. It is commonly known by names such as Tarceva in several regions, with equivalent generics produced under stringent pharmaceutical standards.
2. Medical Uses of Erlocip
2.1 Approved Uses
2.1.1 Non–Small Cell Lung Cancer (NSCLC) Treatment
Erlocip is extensively utilized in the management of NSCLC, particularly in patients whose tumors exhibit EGFR dependency. Its targeted function helps slow tumor progression in advanced cases.
2.1.2 Locally Advanced, Metastatic, or Recurrent NSCLC
The medication is approved for metastatic or recurrent disease, where traditional chemotherapy may offer limited benefits. In such cases, erlotinib offers a more tailored therapeutic strategy.
2.1.3 EGFR Mutation-Positive NSCLC Indications
Patients with activating EGFR mutations—such as exon 19 deletions or exon 21 substitutions—demonstrate enhanced sensitivity to etlotinib. Molecular testing is recommended before initiation.
2.1.4 Pancreatic Cancer (with Gemcitabine Combination)
When combined with gemcitabine, Erlocip enhances treatment outcomes in locally advanced or metastatic pancreatic carcinoma. This combination remains a recognized option in major treatment guidelines.
2.2 Off-Label Uses
2.2.1 Maintenance Therapy After First-Line Chemotherapy
In selected cases, erlotinib is implemented as maintenance therapy to prolong remission following conventional chemotherapeutic regimens.
2.2.2 Head and Neck Squamous Cell Carcinoma
Some clinical investigations support the use of erlotinib in refractory or recurrent head and neck cancers, due to EGFR overexpression in these malignancies.
2.2.3 Colorectal Cancer (EGFR-Dependent Indications)
Although not commonly used, erlotinib has shown exploratory benefits in subsets of colorectal cancer categorized by EGFR-mediated oncogenic signaling.
2.2.4 Ovarian, Renal, and Hepatocellular Carcinoma Investigational Use
Studies continue to evaluate erlotinib for tumors such as ovarian carcinoma, renal cell carcinoma, and hepatocellular carcinoma. Results vary but highlight potential niche benefits.
2.2.5 Brain Metastases in EGFR Mutation-Positive Patients
Erlotinib’s ability to penetrate certain CNS tissues allows exploratory use in patients with EGFR-positive tumors that metastasize to the brain.
3. How Erlocip Works
3.1 Mechanism of Action: EGFR Tyrosine Kinase Inhibition
The medication binds competitively to the ATP-binding site of the EGFR tyrosine kinase, thereby blocking phosphorylation and inhibiting downstream oncogenic pathways.
3.2 Inhibition of Downstream Signaling Pathways
By halting EGFR activation, erlotinib disrupts cascades such as:
- RAS/RAF/MEK/ERK pathway
- PI3K/AKT pathway
- JAK/STAT signaling
These pathways are crucial drivers of malignant cell survival and proliferation.
3.3 Effects on Tumor Cell Proliferation and Apoptosis
Erlocip promotes apoptosis of cancer cells, reduces angiogenesis, and mitigates metastatic spread.
3.4 EGFR Mutation Relevance and Predictive Biomarkers
The presence of activating EGFR mutations predicts a superior therapeutic response. Biomarkers guide clinicians in selecting candidates most likely to benefit.
3.5 Drug Resistance Mechanisms and T790M Mutation
Acquired resistance frequently arises due to secondary mutations such as T790M. This mutation alters the receptor and diminishes erlotinib’s binding affinity.
4. Composition and Formulation
4.1 Active Ingredient: Erlotinib Hydrochloride
The core pharmacological component is erlotinib hydrochloride, supplied in precision-engineered oral tablets.
4.2 Available Strengths and Tablet Formulations
Common strengths include 25 mg, 100 mg, and 150 mg tablets. These allow individualized dosing based on disease severity and patient tolerance.
4.3 Key Excipients and Their Roles
Inactive components support tablet stability, dissolution, and consistency. These excipients ensure proper bioavailability and therapeutic efficacy.
4.4 Packaging and Pharmaceutical Specifications
Erlocip is packaged in moisture-resistant blister packs, maintaining drug integrity throughout storage and transport.
5. Dosage and Administration
5.1 Standard Recommended Dosage for NSCLC
The typical starting dose for NSCLC is 150 mg once daily, administered orally.
5.2 Dosage for Pancreatic Cancer (with Gemcitabine)
For pancreatic carcinoma, 100 mg once daily is recommended alongside gemcitabine infusion therapy.
5.3 Dose Adjustments Based on Liver Function
Hepatic impairment may necessitate dosage modification due to altered metabolism.
5.4 Dose Modifications for Adverse Reactions
Severe rash, diarrhea, or liver abnormalities may require temporary dose reduction or discontinuation.
5.5 How to Take Erlocip: Empty Stomach Requirements
Tablets should be taken at least one hour before meals or two hours after eating to optimize absorption.
5.6 Missed Dose and Vomiting Guidance
If a dose is missed, it should be skipped—no doubling is recommended. Vomiting after a dose does not warrant re-dosing.
5.7 Duration of Treatment and Monitoring
Therapy continues until disease progression or unacceptable toxicity. Periodic imaging and laboratory monitoring are essential.
6. Side Effects of Erlocip
6.1 Overview of Adverse Reaction Profile
Erlocip exhibits a distinct side-effect pattern, often related to EGFR inhibition in normal tissues such as skin and gastrointestinal lining.
6.2 Skin Toxicities and Rash Severity
Acneiform rash is one of the most common effects. Severe cases may progress to dermal ulceration.
6.3 Gastrointestinal Disturbances
Diarrhea, nausea, and abdominal discomfort can occur due to mucosal irritation.
6.4 Ocular Side Effects
Dry eyes, keratitis, and blurred vision may appear, necessitating ophthalmologic evaluation.
6.5 Respiratory Complications (ILD Risk)
Interstitial lung disease (ILD) is rare but potentially life-threatening.
6.6 Hepatic and Renal Impacts
Elevated liver enzymes and renal dysfunction may require intervention.
6.7 Rare But Serious Side Effects
These include corneal perforation, severe blistering reactions, and gastrointestinal bleeding.
7. Common Side Effects
7.1 Acneiform Rash and Dry Skin
Most patients experience dermatologic reactions within the first few weeks.
7.2 Diarrhea and Digestive Symptoms
Hydration and symptomatic therapy help mitigate digestive complaints.
7.3 Fatigue and Weakness
Fatigue may fluctuate and often correlates with disease burden.
7.4 Loss of Appetite and Weight Loss
Anorexia is often reported, requiring nutritional support.
7.5 Hair Changes and Nail Disorders
Brittle nails, alopecia, and hair texture changes may arise.
8. Drug Interactions
8.1 CYP3A4 Interactions: Inducers and Inhibitors
Drugs affecting CYP3A4 can significantly alter erlotinib plasma concentrations.
8.2 Proton Pump Inhibitors and Acid-Reducing Agents
Reduced stomach acidity can impair absorption, reducing therapeutic efficacy.
8.3 Warfarin and Anticoagulants
Erlocip may potentiate anticoagulant effects, increasing bleeding risk.
8.4 Antibiotics, Antifungals, and Antivirals
Many of these medications influence hepatic enzyme pathways and warrant caution.
8.5 Smoking Interaction: Effect on Drug Levels
Smoking accelerates erlotinib metabolism, lowering drug concentrations and diminishing effectiveness.
8.6 Food, Herbal, and Supplement Interactions
Herbal agents like St. John’s Wort and certain supplements may disrupt drug kinetics.
9. Warnings and Important Precautions
9.1 Severe Skin Reactions and Stevens–Johnson Syndrome
Rare but critical dermatologic events require immediate medical intervention.
9.2 Interstitial Lung Disease (ILD) Warning
Any new respiratory symptoms warrant urgent evaluation for ILD.
9.3 Hepatotoxicity Precautions
Frequent monitoring of liver enzymes is advised during therapy.
9.4 Gastrointestinal Perforation Risk
The risk increases in patients with prior peptic ulcers or concomitant steroid use.
9.5 Cardiovascular and Renal Considerations
Exacerbation of pre-existing cardiac or renal disease may occur.
9.6 Photosensitivity Precautions
Sun protection is essential due to heightened sensitivity to UV radiation.
9.7 Smoking Cessation Advice for Effectiveness
Patients are strongly advised to discontinue smoking to maintain therapeutic plasma levels.
10. Contraindications
10.1 Absolute Contraindications
Erlotinig therapy must not be initiated in individuals with specific medical exclusions. Absolute contraindications exist to prevent severe, life-threatening outcomes. These include:
- Documented severe hypersensitivity reactions to erlotinib.
- History of life-threatening dermatologic reactions linked to EGFR inhibitors.
- Situations where the benefit–risk ratio is unequivocally unfavorable.
10.2 Hypersensitivity to Erlotinib or Excipients
Any patient with known hypersensitivity to erlotinib or any component contained within the formulation should strictly avoid therapy. Reactions may range from mild urticaria to fulminant anaphylaxis. Even minimal exposure may precipitate systemic inflammatory responses.
10.3 Conditions Requiring Therapy Avoidance
Certain medical conditions necessitate avoidance of treatment due to heightened vulnerability:
- Severe hepatic failure.
- Ongoing active gastrointestinal perforation.
- Uncontrolled pulmonary fibrosis or similar respiratory compromise.
These conditions dramatically increase the risk of fatal complications.
11. Careful Administration
11.1 Pre-Existing Liver or Kidney Disorders
Patients with impaired hepatic or renal function warrant meticulous monitoring. Altered drug metabolism may result in heightened serum concentrations, increasing toxicity. Dose titration may be necessary to navigate fluctuating organ function.
11.2 Patients with Pulmonary Conditions
Those with pulmonary disorders such as chronic interstitial pneumonitis or chronic obstructive respiratory diseases face elevated risks. Erlotinib has been associated with interstitial lung disease-like events. Sudden respiratory changes require immediate evaluation.
11.3 Patients Receiving Anticoagulants
Co-administration with warfarin or other anticoagulants may potentiate bleeding tendencies. INR levels can destabilize unexpectedly. Frequent monitoring is essential to prevent hemorrhagic episodes.
11.4 Immunocompromised or Frail Patients
Fragile or immunosuppressed individuals may experience amplified adverse effects. Susceptibility to infections, dermatologic complications, and metabolic instability is substantially increased.
11.5 Concomitant Use with Chemotherapy or Radiation
Concurrent chemoradiation escalates toxicity risks, including mucositis, pneumonitis, and severe integumentary reactions. Combination therapy should be approached with caution and continuous assessment.
12. Use in Special Populations
12.1 Administration to Elderly
12.1.1 Adjustments and Increased Monitoring
Elderly patients may require individualized dosage regimens due to diminished physiological reserves. Routine clinical assessments help ensure safe, sustained therapy.
12.1.2 Expected Adverse Event Patterns
Older adults may exhibit more pronounced fatigue, dermatologic events, and gastrointestinal discomfort. These patterns must be anticipated when planning long-term treatment.
12.2 Administration to Pregnant Women
12.2.1 Embryotoxic and Teratogenic Risks
Animal studies indicate embryo–fetal toxicity and potential malformation risks. Fetal exposure may interfere with developmental pathways controlled by EGFR signaling.
12.2.2 Pregnancy Category and Risk Summary
Erlotinib is classified as a high-risk medication in pregnancy. Initiation during gestation is strongly discouraged unless no alternative therapy exists and benefits outweigh risks.
12.3 Administration to Nursing Mothers
12.3.1 Drug Transfer Into Breast Milk
Erlotinib and its metabolites may be excreted in human milk, posing potential cytotoxic risks to infants. Even trace levels may be harmful due to immature metabolic pathways.
12.3.2 Breastfeeding Discontinuation Guidance
Nursing should be discontinued prior to beginning therapy. Alternative feeding methods are advised throughout the treatment period.
12.4 Administration to Children
12.4.1 Safety and Efficacy in Pediatric Cancer
Pediatric data remain limited. While certain trials explore use in pediatric malignancies, consistent safety profiles have not been established.
12.4.2 Pediatric Dose Considerations
Dosing for children must be approached cautiously due to metabolic unpredictability. Adjustments must reflect body surface area, organ maturity, and therapeutic response.
13. Overdosage
13.1 Symptoms of Acute Overdose
Acute overdose can precipitate severe dermatologic reactions, intense diarrhea, hepatotoxicity, and profound fatigue. Symptoms may escalate rapidly.
13.2 Management and Supportive Care
There is no specific antidote. Management includes:
- Immediate discontinuation of therapy.
- Hydration and electrolyte correction.
- Symptom-directed medical care.
13.3 Emergency Monitoring Requirements
Continuous monitoring of vital signs, hepatic enzymes, and renal function is required until stabilization. Hospitalization is often warranted.
14. Handling and Storage
14.1 Recommended Storage Conditions
Erlotinib tablets should be stored at controlled room temperatures, typically between 20°C and 25°C. Extreme conditions may degrade potency.
14.2 Light, Moisture, and Temperature Sensitivity
The medication is susceptible to humidity and direct light. Protection within original packaging ensures medicinal integrity.
14.3 Safe Handling Procedures for Cytotoxic Drugs
As a cytotoxic agent, erlotinib requires careful handling. Tablets should not be crushed or split. Contact with dust or residue must be avoided.
14.4 Disposal Guidelines for Unused Medication
Unused tablets must be disposed of following local cytotoxic waste regulations. Household disposal is strongly discouraged.
14.5 Pharmacy and Home Storage Considerations
Both clinical and home environments should ensure secure storage out of reach of children, pets, and unauthorized individuals.
15. Handling Precautions
15.1 Care for Caregivers and Healthcare Providers
Those administering or assisting with the medication must avoid direct contact with tablets. Proper hygiene and handling protocols minimize exposure.
15.2 Use of Gloves and Protective Equipment
Protective gloves are recommended when touching packaging or assisting patients. This reduces dermal or accidental ingestion risks.
15.3 Avoiding Tablet Crushing or Breaking
Tablet manipulation increases exposure to cytotoxic material. Whole-tablet ingestion is mandatory.
15.4 Preventing Environmental Exposure
Contaminated materials—blister packs, gloves, or wipes—should be discarded safely. Environmental contamination must be prevented at all times.
15.5 Transportation and Compliance Precautions
During transport, tablets must remain sealed within original blisters. Compliance with pharmaceutical safety regulations ensures safe delivery and storage.