1. Introduction to Nimodip and Nimodipine
1.1 Overview of Nimodipine as a Calcium Channel Blocker
Nimodipine is a dihydropyridine calcium channel antagonist engineered to exert a preferential vasodilatory effect on cerebral vasculature. Its distinctive ability to modulate calcium influx in smooth muscle cells contributes to enhanced perfusion in delicate neurological tissues.
1.2 Pharmacological Classification and Therapeutic Importance
Classified under selective L-type calcium channel blockers, nimodipine occupies a vital position in neurovascular medicine. Its clinical value is driven by:
- Superior penetration across the blood–brain barrier
- Protection of vulnerable neuronal structures
- Reduction of delayed ischemic deficits post-hemorrhagic injury
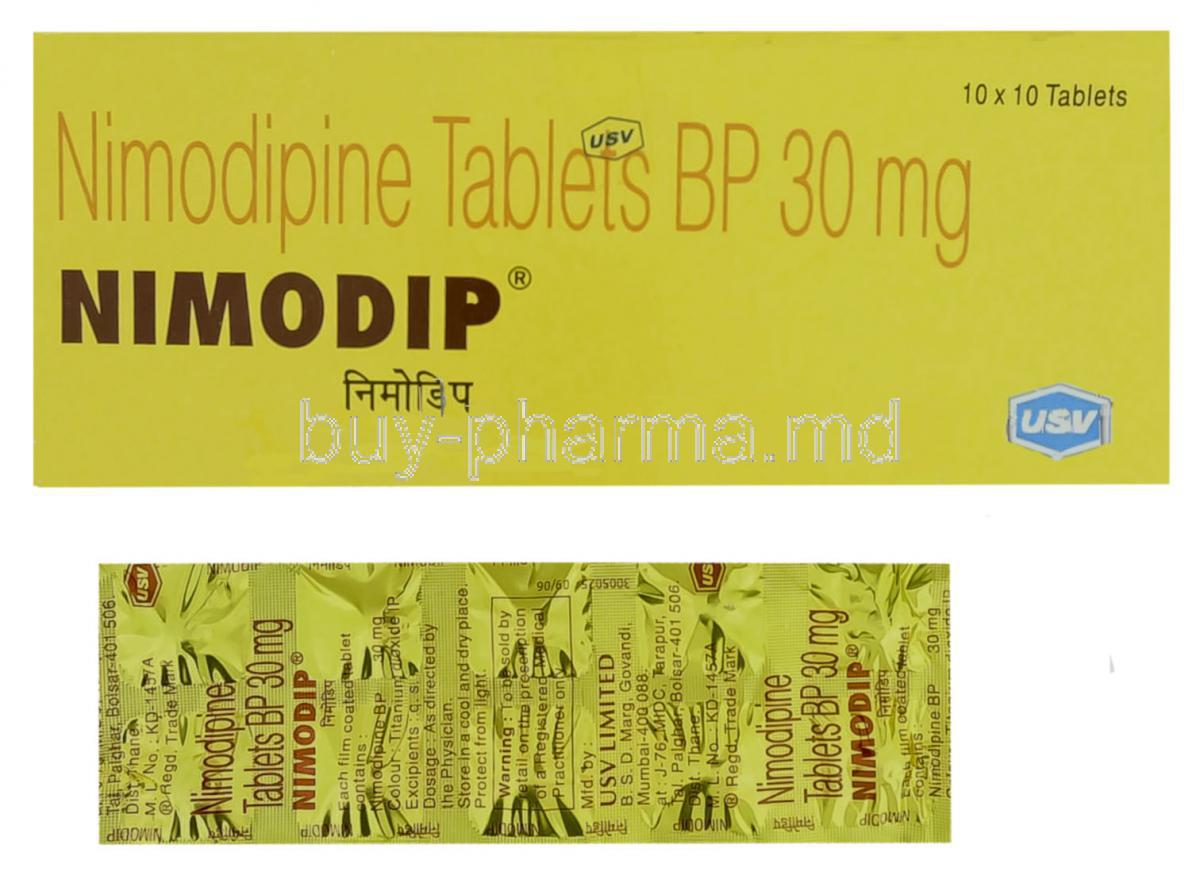
1.3 Key Differences Between Nimodip® Brand and Generic Nimodipine
Both the branded Nimodip® and its generic equivalents contain identical therapeutic constituents. However, distinctions may arise in excipient composition, dissolution profiles, and packaging integrity. These subtle variations may influence tolerability in a small subset of patients, though clinical efficacy remains equivalent.
1.4 Role of Nimodipine in Neurological and Vascular Protection
Nimodipine plays a pivotal role in safeguarding neuronal health. By enhancing microcirculatory flow and minimizing vasospasm-induced ischemia, it effectively supports structural and functional preservation of the brain’s delicate tissues.
2. Composition and Formulation
2.1 Active Ingredient: Nimodipine
The primary therapeutic agent is nimodipine, a potent and lipophilic calcium channel blocker designed for targeted cerebral activity.
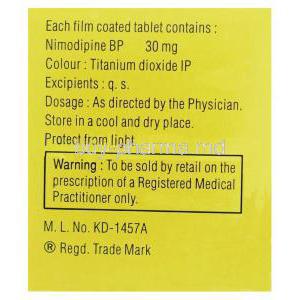
2.2 Mechanism-Enhancing Excipients
Pharmaceutical formulations include solubilizers, stabilizers, and absorption-enhancing excipients. These auxiliary ingredients improve dissolution, sustain potency, and optimize the delivery of nimodipine into systemic circulation.
2.3 Available Dosage Forms (Tablets, Capsules, Oral Solution)
Nimodipine is commonly dispensed as:
- Soft gelatin capsules
- Immediate-release tablets
- Oral liquid formulations for patients with swallowing difficulties
2.4 Bioavailability Considerations of Oral vs. Alternative Formulations
Oral nimodipine exhibits variable bioavailability influenced by hepatic first-pass metabolism. Liquid preparations often provide more predictable absorption, while capsule forms are valued for ease of administration and stability.
3. How Nimodipine Works
3.1 Mechanism of Action: Calcium Channel Blockade in Cerebral Arteries
Nimodipine selectively inhibits voltage-dependent calcium channels, preventing calcium overload in vascular smooth muscle. This induces relaxation of cerebral arteries and augments blood distribution within ischemic zones.
3.2 Reduction of Cerebral Vasospasm and Neuroprotection
By attenuating vasospasm—a major complication after subarachnoid hemorrhage—nimodipine alleviates ischemic stress. This protective effect reduces secondary neurological injuries and improves functional outcomes.
3.3 Hemodynamic Effects and Vascular Selectivity
Unlike systemic vasodilators, nimodipine demonstrates high affinity for cerebral vessels, minimizing widespread hypotension. This selectivity ensures:
- Enhanced cerebral perfusion
- Minimal peripheral vascular disruption
- Greater neurological benefit
3.4 Impact on Intracellular Calcium Levels and Neuronal Health
Lower intracellular calcium levels mitigate excitotoxicity, a major contributor to neuronal apoptosis. Nimodipine thereby supports neuronal resilience during vascular compromise.
4. Therapeutic Uses
4.1 Primary Use: Prevention and Treatment of Cerebral Vasospasm
Nimodipine remains the gold-standard therapy for preventing and alleviating vasospasm following aneurysmal subarachnoid hemorrhage. This intervention is crucial for minimizing delayed cerebral ischemia.
4.2 Management of Neurological Deficits Following Subarachnoid Hemorrhage (SAH)
Patients recovering from SAH often experience cognitive and motor impairments. Nimodipine enhances neurological recovery by stabilizing regional blood flow and reducing ischemia-induced damage.
4.3 Improving Cerebral Blood Flow in Vascular-Related Cognitive Impairment
Impaired microcirculation contributes to cognitive decline. Nimodipine may ameliorate attention deficits, memory disturbances, and executive dysfunction by improving cerebral perfusion dynamics.
4.4 Adjunct Use in Acute Stroke Management
Although not universally indicated, nimodipine may be used adjunctively in certain stroke management protocols to reduce vasospastic complications and optimize cerebral perfusion.
5. Off-Label Uses
5.1 Migraine Prophylaxis and Headache Disorders
Nimodipine has demonstrated benefit in select headache syndromes due to its vasodilatory and neurostabilizing properties.
5.2 Raynaud’s Syndrome and Peripheral Vasospastic Disorders
The drug’s ability to modulate vascular tone has led to off-label use in reducing vasospastic episodes in Raynaud’s phenomenon.
5.3 Management of Cognitive Dysfunction in Dementia-Related Circulatory Issues
Enhanced microvascular perfusion may support brain function in patients with vascular dementia or circulatory-driven cognitive decline.
5.4 Adjunctive Use in Organ Transplant Perfusion and Cellular Protection
Nimodipine may be applied to improve organ preservation and cellular viability during transplantation procedures.
5.5 Use in High-Altitude Cerebral Edema (HACE) Prevention
Its vasodilatory effects provide theoretical benefit in mitigating high-altitude cerebral complications.
6. Dosage and Administration
6.1 Standard Adult Dosage for SAH-Related Vasospasm
The widely adopted regimen involves administering nimodipine 60 mg every four hours for a 21-day therapeutic cycle.
6.2 Recommended Titration Schedule and Duration of Therapy
Titration is tailored based on blood pressure response. Slow upward adjustments are advised in individuals prone to hypotension.
6.3 Administration via Oral Capsule and Handling Precautions
Capsules should be swallowed whole. Opening or injecting capsule contents is contraindicated due to risk of severe systemic hypotension.
6.4 Timing of Doses Relative to Food and Other Medications
Consistency is essential. Nimodipine may be taken with or without food, but spacing from interacting drugs—particularly CYP3A4 modulators—is critical.
6.5 Missed Dose Guidelines and Adjustments Based on Clinical Response
A missed dose should be taken promptly unless close to the next scheduled intake. Double dosing is not recommended.
7. Warnings and Important Precautions
7.1 Risk of Severe Hypotension and Hemodynamic Instability
Nimodipine can precipitate clinically significant hypotension. Vigilant hemodynamic monitoring is mandatory.
7.2 Liver Function Impairment and Required Monitoring
Reduced hepatic clearance heightens systemic exposure. Periodic liver function assessments are advised.
7.3 Caution in Patients with Intracranial Pressure Disorders
Fluctuations in vascular tone may exacerbate intracranial pressure variations, requiring cautious administration.
7.4 Contraindication in Intravenous Administration of Oral Formulations
Oral nimodipine must never be injected. Such misuse may provoke life-threatening circulatory collapse.
7.5 Drug-Induced Dizziness and Impact on Ability to Drive or Operate Machinery
Dizziness, somnolence, and slowed reaction times necessitate caution in hazardous activities.
8. Contraindications
8.1 Known Hypersensitivity to Nimodipine or Formulation Components
Hypersensitive individuals should avoid nimodipine to prevent adverse immunological reactions.
8.2 Clinically Significant Hypotension
Patients with untreated or profound hypotension should not initiate therapy.
8.3 Concomitant Use with Strong CYP3A4 Inhibitors
Potent inhibitors dramatically elevate drug plasma levels, risking toxicity.
8.4 Severe Hepatic Impairment and Drug Metabolism Concerns
Marked hepatic dysfunction compromises metabolism and increases adverse event risk.
9. Careful Administration and Patient Monitoring
9.1 Monitoring Blood Pressure and Pulse
Frequent monitoring ensures early detection of undue cardiovascular responses.
9.2 Assessment for Signs of Cerebral Edema or Neurological Decline
Regular neurological evaluations are essential for timely management of complications.
9.3 Adjustments in Patients with Renal or Hepatic Dysfunction
Dose reductions or extended intervals may be required to prevent accumulation.
9.4 Monitoring for Drug Accumulation During Long-Term Use
Observation for prolonged sedation, hypotension, or cognitive decline helps identify potential overexposure.
10. Side Effects
10.1 Overview of Adverse Reaction Profile
Nimodipine, like other calcium channel antagonists, possesses a distinct adverse reaction spectrum. While many side effects are mild and transient, others may manifest with greater severity depending on individual susceptibility or concurrent medical conditions. The pharmacodynamic influence on vascular tone, cardiac conduction, and neurological pathways contributes to a broad array of potential reactions. Some events appear early in therapy, whereas others emerge with prolonged exposure.
10.2 Frequency and Severity of Cardiovascular Reactions
Cardiovascular responses are among the most frequently reported with nimodipine. These effects stem primarily from peripheral vasodilation and altered hemodynamic stability.
- Episodes of reduced blood pressure, occasionally profound
- Compensatory tachycardia or reflexive changes in heart rate
- Mild peripheral edema linked to reduced vascular resistance
Although most reactions remain manageable, severe hypotension may require urgent dose modification or cessation.
10.3 Neurological and Gastrointestinal Side Effects
Neurological reactions may include headaches, dizziness, or transient disorientation due to fluctuations in cerebral perfusion. Gastrointestinal events—though usually mild—can disrupt adherence.
- Constipation, nausea, or abdominal discomfort
- Occasional episodes of vomiting or reduced appetite
- Mood fluctuations or subtle cognitive fog in sensitive individuals
10.4 Rare but Serious Adverse Events (Anaphylaxis, Severe Hypotension)
Although uncommon, serious reactions demand immediate medical intervention:
- Anaphylactic responses characterized by airway swelling, rash, or circulatory collapse
- Critical hypotension leading to fainting, confusion, or organ underperfusion
- Profound bradycardia with compromised cardiac output
11. Common Side Effects
11.1 Headache and Lightheadedness
Headache remains one of the most characteristic complaints. It often arises due to sudden vasodilation in cerebral vessels. Lightheadedness may accompany positional changes or early dosing phases.
11.2 Flushing and Warm Sensation
Flushing occurs as superficial blood vessels dilate. Patients often describe a transient warmth across the face, neck, or upper chest, usually resolving without intervention.
11.3 Tachycardia or Palpitations
A rapid heartbeat may emerge as the body attempts to compensate for lowered vascular resistance. These palpitations are generally benign but may feel unsettling.
11.4 Nausea, Abdominal Discomfort, and Mild Edema
Nausea and digestive unease can develop early during treatment. Mild swelling in the extremities may result from fluid shifts associated with peripheral vasodilation.
11.5 Fatigue and Weakness
Generalized tiredness may occur as a result of decreased blood pressure or metabolic adaptation to the medication. Symptoms often lessen with continued use.
12. Drug Interactions
12.1 CYP3A4 Inhibitors (Macrolide Antibiotics, Azole Antifungals, HIV Medications)
Strong CYP3A4 inhibitors significantly elevate nimodipine concentrations by slowing its hepatic metabolism. This may provoke exaggerated hypotensive or neurological effects.
12.2 CYP3A4 Inducers (Rifampin, Phenytoin, Carbamazepine)
Inducers accelerate metabolic clearance of nimodipine, reducing therapeutic efficacy. Dose adjustments or alternative therapies may be required.
12.3 Interactions with Antihypertensive Medications
Concomitant use with other antihypertensives may precipitate excessive blood pressure reductions. Monitoring and cautious titration are essential.
12.4 Effects of Grapefruit Juice on Drug Levels
Grapefruit compounds inhibit intestinal CYP3A4, dramatically increasing systemic exposure. Avoidance of grapefruit products is strongly recommended.
12.5 Interactions with Sedatives, Alcohol, and CNS Depressants
Co-administration with depressant agents may intensify dizziness, lethargy, or coordination impairment, increasing the risk of accidents or falls.
13. Administration to Specific Populations
13.1 Elderly Patients
13.1.1 Increased Sensitivity to Hypotension
Elderly individuals often demonstrate heightened susceptibility to blood pressure fluctuations, requiring conservative dosing and vigilant observation.
13.1.2 Adjusted Monitoring Protocols
Frequent hemodynamic assessments help prevent complications. Elderly patients may require longer intervals between dose adjustments.
13.1.3 Fall Risk and Cognitive Considerations
Lightheadedness and slower reflexes increase fall risk. Cognitive changes must also be monitored, as subtle impairment may appear during therapy.
13.2 Pregnant Women
13.2.1 Safety Data and Fetal Risk Assessment
Human data remain limited. Potential risks must be weighed carefully against therapeutic benefits, especially in conditions where cerebral perfusion is compromised.
13.2.2 Placental Transfer and Teratogenicity Concerns
Nimodipine may cross the placenta. Although no definitive teratogenic patterns are established, use during pregnancy requires stringent medical oversight.
13.3 Nursing Mothers
13.3.1 Excretion into Breast Milk
Small quantities may transfer into breast milk, potentially affecting the nursing infant’s cardiovascular or neurological stability.
13.3.2 Infant Exposure Risks and Recommendations
Breastfeeding decisions should consider alternative feeding options when maternal therapy cannot be interrupted.
13.4 Children and Adolescents
13.4.1 Lack of Established Safety and Efficacy
Clinical trials in pediatric groups are limited. As a result, routine use is not recommended without compelling indications.
13.4.2 Special Monitoring if Off-Label Pediatric Use is Considered
In rare cases where nimodipine is used for specialized indications, close cardiovascular and neurological monitoring is mandatory.
14. Overdosage
14.1 Expected Clinical Presentation of Nimodipine Toxicity
Overdose manifestations typically include profound hypotension, severe dizziness, and cardiovascular instability. Neurological depression or confusion may also appear.
14.2 Severe Hypotension, Bradycardia, and Cardiac Suppression
Extreme vasodilation may suppress cardiac output. Bradycardia or atrioventricular conduction disturbances can complicate the clinical picture.
14.3 Emergency Management and Supportive Care Strategies
Immediate intervention includes:
- Intravenous fluid resuscitation
- Vasopressor administration when indicated
- Continuous cardiac monitoring and airway support
14.4 Role of Activated Charcoal and Hemodynamic Stabilization
Activated charcoal may reduce absorption when administered promptly. Hemodynamic stabilization is prioritized to prevent organ hypoperfusion.
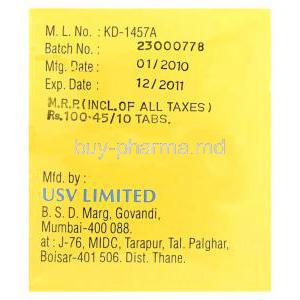
15. Handling and Storage
15.1 Recommended Storage Temperature and Light Protection
Nimodipine requires storage at controlled room temperature, shielded from direct light to preserve molecular integrity.
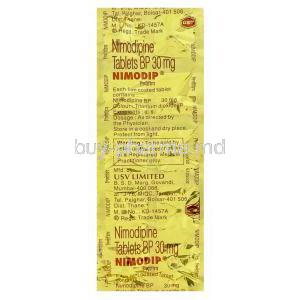
15.2 Importance of Keeping Capsules in Blister to Avoid Degradation
The blister packaging protects each capsule from humidity and oxidation. Premature removal may degrade potency.
15.3 Safe Handling Instructions for Healthcare Providers
Healthcare personnel should avoid excessive heat exposure during storage and ensure accurate dispensing to prevent administration errors.
15.4 Stability Considerations After Opening Packaging
Once opened, capsules should be used promptly to avoid environmental degradation that may impair therapeutic effectiveness.
16. Handling Precautions
16.1 Avoiding Intravenous Administration Errors
Oral formulations must never be injected. Inadvertent IV use can trigger catastrophic cardiovascular collapse.
16.2 Prevention of Accidental Overexposure During Hospital Use
Clear labeling and segregated storage help prevent mix-ups. Staff training reduces risk of dosing or route-of-administration errors.
16.3 Safety Measures When Splitting or Manipulating Capsules
Capsules are not designed for splitting. Manipulation may alter absorption characteristics or lead to dose inconsistencies.
16.4 Disposal of Expired or Unused Nimodipine
Unused or outdated medication should be discarded following pharmaceutical waste protocols to prevent accidental ingestion or environmental contamination.