1. Introduction
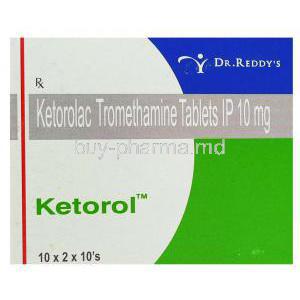
Overview of Ketorol and Ketorolac
Ketorol, known generically as Ketorolac, is a potent nonsteroidal anti-inflammatory drug (NSAID) widely prescribed for the short-term relief of moderate to severe pain. Unlike opioids, it provides effective analgesia without the risk of dependency. Its primary role lies in postoperative and acute pain management across various medical disciplines.
Classification: Nonsteroidal Anti-Inflammatory Drug (NSAID)
Belonging to the heteroaryl acetic acid derivative class of NSAIDs, Ketorolac exerts multifaceted pharmacological actions — analgesic, anti-inflammatory, and antipyretic. It is frequently chosen for its opioid-sparing properties, allowing reduced reliance on narcotic medications in acute care settings.
Brand Names and Generic Availability
Marketed under brand names such as Ketorol, Toradol, Acular, and Sprix, Ketorolac is globally available in multiple formulations. Its generic equivalents have ensured broader accessibility and cost-effectiveness in both hospital and outpatient environments.
Therapeutic Class and Pharmacological Profile
Ketorolac falls under the therapeutic class of analgesic anti-inflammatory agents. It provides systemic relief by inhibiting prostaglandin synthesis, a biochemical mediator of pain and inflammation. Its profile encompasses rapid onset and predictable duration of action, making it a preferred option in surgical recovery and emergency care.
Historical Background and Clinical Approval
Developed in the late 1980s, Ketorolac gained regulatory approval as one of the first injectable NSAIDs for postoperative pain. Since then, it has remained a cornerstone in multimodal analgesia protocols worldwide, emphasizing efficacy balanced with cautious short-term use.
2. Composition and Active Ingredients
Chemical Composition and Formulation
The active moiety, Ketorolac tromethamine, is a white crystalline compound with strong solubility in water and ethanol. Its molecular formula is C15H13NO3, and its structure facilitates rapid absorption and bioavailability across various delivery routes.
Available Dosage Forms
- Tablets for oral administration (10 mg)
- Intramuscular and intravenous injections (30 mg/mL)
- Ophthalmic drops for ocular inflammation
- Nasal spray for rapid systemic analgesia
Excipients and Formulation Differences
Inactive ingredients such as sodium chloride, ethanol, and benzalkonium chloride vary depending on the route of administration. Ophthalmic and parenteral forms are specifically designed to minimize irritation and maintain isotonicity.
Manufacturer Variations Across Global Markets
Ketorol is produced by multiple pharmaceutical entities including Dr. Reddy’s, Sun Pharma, and Roche. Formulation standards may differ regionally due to pharmacopeial regulations, though all adhere to stringent quality control protocols.
3. Mechanism of Action (How Ketorol Works)
COX Inhibition and Prostaglandin Suppression
Ketorolac acts by reversibly inhibiting cyclooxygenase (COX-1 and COX-2) enzymes, thereby suppressing the synthesis of prostaglandins. These mediators are pivotal in transmitting pain signals, inducing inflammation, and elevating body temperature.
Analgesic, Anti-inflammatory, and Antipyretic Actions
Through prostaglandin blockade, Ketorolac delivers tri-modal efficacy:
- Analgesic: Rapid reduction of acute pain intensity
- Anti-inflammatory: Decreased tissue swelling and joint stiffness
- Antipyretic: Lowering elevated body temperature
Pharmacodynamics and Duration of Effect
The drug achieves peak plasma concentration within 30–60 minutes after oral or intramuscular administration. Its half-life averages 4–6 hours, ensuring sustained analgesia with predictable clearance through renal pathways.
Onset of Analgesic Activity
In most patients, pain relief begins within 30 minutes post-dose. Injectable forms exhibit the fastest onset, followed by nasal spray and oral formulations, offering tailored options for both clinical and ambulatory pain control.
4. Approved Medical Uses
- Short-term management of moderate to severe acute pain
- Control of postoperative pain in surgical, dental, or orthopedic procedures
- Treatment of musculoskeletal disorders and soft tissue injuries
- Relief of renal colic and acute migraine attacks
- Ophthalmic use in reducing inflammation after cataract or corneal surgery
5. Off-Label Uses
Beyond its primary indications, Ketorolac is also employed in:
- Cancer-related pain management as part of palliative regimens
- Fracture and trauma-associated pain to minimize opioid requirements
- Dysmenorrhea and other gynecologic pain syndromes
- Gout flares and inflammatory arthropathies
- Emergency medicine for acute pain control protocols
- Adjunct therapy in multimodal analgesic approaches
6. Dosage and Administration
6.1 Dosage Guidelines
For adults, the usual oral dose is 10 mg every 4–6 hours as needed, not exceeding 40 mg daily. Injectable administration ranges from 30 mg IM/IV every 6 hours, with a maximum total duration of 5 days to minimize renal and gastrointestinal risks. Patients with renal impairment or low body weight require dose reduction.
6.2 Administration Instructions
- Oral: Take with water, preferably after meals to minimize gastric discomfort.
- Injection: Administer slowly IM or IV under medical supervision.
- Ophthalmic: Instill drops without touching the tip to the eye surface.
- Nasal spray: Use as directed, one spray per nostril for rapid systemic absorption.
7. Important Precautions
- Therapy should not exceed 5 consecutive days for systemic use.
- Monitor renal, hepatic, and gastrointestinal function during therapy.
- Avoid concomitant use with other NSAIDs or anticoagulants.
- Patients with peptic ulcer history require special caution.
8. Contraindications
- Active or prior gastrointestinal bleeding or ulceration
- Known hypersensitivity to Ketorolac or related NSAIDs
- Severe renal impairment or dehydration
- Use during labor, delivery, or perioperative CABG procedures
- History of NSAID-induced bronchospasm or asthma
9. Warnings and Black Box Alerts
- Gastrointestinal risk: Potential for ulcers, bleeding, or perforation
- Cardiovascular risk: May increase risk of stroke or myocardial infarction
- Renal toxicity: Monitor for reduced urine output or elevated creatinine
- Hemorrhagic complications: Avoid in patients with bleeding disorders
- Allergic reactions: Rare anaphylaxis and bronchospasm may occur
- Pregnancy risk: Avoid during late pregnancy due to fetal circulatory effects
10. Common and Serious Side Effects
10.1 Common Side Effects
- Nausea and vomiting
- Dizziness or somnolence
- Headache and abdominal discomfort
- Mild irritation at injection site
10.2 Serious Side Effects
- Severe gastrointestinal bleeding or ulcer formation
- Renal dysfunction or acute failure
- Hypertension, fluid retention, or edema
- Anaphylactic or hypersensitivity reactions
- Visual impairment in ophthalmic formulations
11. Drug Interactions
Interaction with Anticoagulants (Warfarin, Heparin)
Ketorolac may potentiate the anticoagulant effects of warfarin, heparin, and similar agents. This interaction heightens the risk of spontaneous bleeding, hematoma formation, or prolonged clotting time. Patients on concurrent therapy should undergo frequent monitoring of coagulation parameters and clinical assessment for bruising, hematuria, or gastrointestinal bleeding.
Antihypertensive Agents (ACE Inhibitors, ARBs, Diuretics)
When combined with angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), or diuretics, Ketorolac may diminish antihypertensive efficacy and exacerbate renal dysfunction. NSAIDs can attenuate renal prostaglandin-mediated vasodilation, particularly in volume-depleted or elderly patients. Regular blood pressure and renal function evaluation is essential.
Other NSAIDs and Corticosteroids
Concurrent administration with other NSAIDs or corticosteroids markedly increases gastrointestinal toxicity. The synergistic inhibition of protective gastric prostaglandins can result in ulcers, perforation, or bleeding. Combined use should be avoided unless absolutely necessary and under direct medical supervision.
Lithium and Methotrexate Toxicity Risk
Ketorolac interferes with the renal clearance of lithium and methotrexate, leading to potential toxicity. Elevated serum levels can provoke nephrotoxicity, hepatotoxicity, or neurotoxicity. Dose adjustments and close serum concentration monitoring are warranted when used concomitantly.
SSRIs and Increased Bleeding Tendency
Co-administration with selective serotonin reuptake inhibitors (SSRIs) such as sertraline or fluoxetine can increase bleeding risk through platelet function inhibition. Caution is advised in individuals with bleeding disorders, gastrointestinal disease, or concurrent anticoagulant therapy.
Alcohol and Gastrointestinal Complications
Alcohol intensifies gastrointestinal irritation associated with Ketorolac, amplifying the likelihood of mucosal erosion and ulceration. Patients should be strongly counseled to avoid alcohol consumption during therapy to minimize gastric injury and hepatic strain.
12. Use in Special Populations
12.1. Elderly Patients
Elderly individuals exhibit heightened pharmacodynamic sensitivity to Ketorolac’s adverse effects, particularly gastrointestinal bleeding and renal impairment. Lower initial doses, limited duration of therapy, and frequent renal and hepatic function tests are recommended.
- Start with the minimal effective dose
- Monitor for fluid retention or gastrointestinal distress
- Evaluate renal output and serum creatinine regularly
12.2. Pregnant and Nursing Women
Ketorolac is classified as Category C in early pregnancy and Category D in the third trimester due to fetal cardiovascular and renal complications. It may induce premature closure of the ductus arteriosus and reduce amniotic fluid volume. The drug passes into breast milk in trace amounts, necessitating either discontinuation of breastfeeding or substitution of therapy.
- Contraindicated during late pregnancy
- Use only if benefits outweigh fetal risk in earlier trimesters
- Avoid during lactation whenever possible
12.3. Pediatric Administration
Use in children is limited to specific clinical settings such as postoperative pain management under strict supervision. Dosing is calculated by body weight, typically 0.5 mg/kg per administration, not exceeding adult maximums. Continuous observation for gastrointestinal irritation and renal dysfunction is essential.
13. Careful Administration and Monitoring
Ketorolac demands vigilant oversight in patients with underlying conditions or concurrent pharmacotherapy. Risk-benefit assessment should precede prescription in the following scenarios:
- Renal or hepatic impairment: Reduced metabolism and elimination increase systemic exposure.
- History of gastrointestinal disease: Higher susceptibility to ulcer recurrence and bleeding.
- Concurrent anticoagulant or corticosteroid use: Amplified hemorrhagic and mucosal risk.
- Cardiovascular disorders: Potential fluid retention and blood pressure elevation.
- Asthma or NSAID allergy: Risk of bronchospasm or hypersensitivity reactions.
14. Overdosage
Excessive intake of Ketorolac can result in toxic manifestations such as nausea, vomiting, abdominal pain, drowsiness, and lethargy. Severe intoxication may precipitate metabolic acidosis, renal failure, and gastrointestinal hemorrhage.
- Immediate medical attention is imperative.
- Management is largely supportive and symptomatic.
- Gastric lavage or administration of activated charcoal may aid decontamination if performed promptly.
- Forced diuresis and dialysis offer limited benefit due to high protein binding.
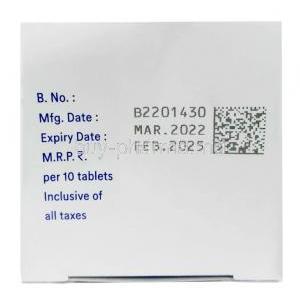
15. Handling and Storage
- Store at controlled room temperature (15–30°C).
- Protect from light, moisture, and excessive heat exposure.
- Keep injectable and ophthalmic solutions in tightly sealed containers.
- Discard opened or expired vials following institutional safety guidelines.
- Healthcare personnel should wear gloves when handling parenteral forms to prevent dermal contact.
16. Clinical Pharmacokinetics
Ketorolac is rapidly absorbed following oral or intramuscular administration, exhibiting bioavailability above 85%. Food may delay peak absorption but does not reduce overall systemic exposure.
- Distribution: Approximately 99% bound to plasma proteins, primarily albumin.
- Metabolism: Extensively hepatically metabolized via glucuronidation.
- Excretion: Predominantly renal (about 90%) with minor biliary clearance.
- Half-life: 4–6 hours in healthy adults; prolonged in elderly or renal-impaired individuals.
17. Patient Education and Counseling
Patients should be informed about responsible use and early detection of adverse effects. Education enhances adherence and minimizes risks.
- Follow prescribed dose and duration; do not exceed 5 days of systemic therapy.
- Take medication after meals with water to reduce gastric irritation.
- Report any signs of bloody stools, persistent abdominal pain, or reduced urine output immediately.
- Maintain adequate hydration throughout treatment.
- Avoid alcohol and unnecessary use of other NSAIDs.
- Seek medical care for prolonged pain, dizziness, or allergic manifestations.
18. Summary and Key Takeaways
Ketorolac remains a highly effective agent for short-term pain relief, especially in postoperative and acute care scenarios. Its use demands precision, restraint, and vigilant monitoring to prevent systemic complications.
- Demonstrates potent analgesia without narcotic dependency.
- Requires awareness of gastrointestinal, renal, and cardiovascular safety.
- Individualized dosing and medical oversight ensure therapeutic success.
- For chronic or persistent pain, alternative therapies should be considered under professional guidance.