Introduction to Cefadur (Cefadroxil)
Cefadur, containing the active pharmaceutical ingredient cefadroxil, is a well-established antibacterial agent widely prescribed for the management of various bacterial infections. Classified as a first-generation cephalosporin antibiotic, it is valued for its broad spectrum of activity and favorable safety profile. This medication is available by prescription in most countries and plays a critical role in the eradication of susceptible bacterial pathogens. By targeting specific bacterial structures, Cefadur assists in restoring patient health and preventing complications associated with untreated infections.
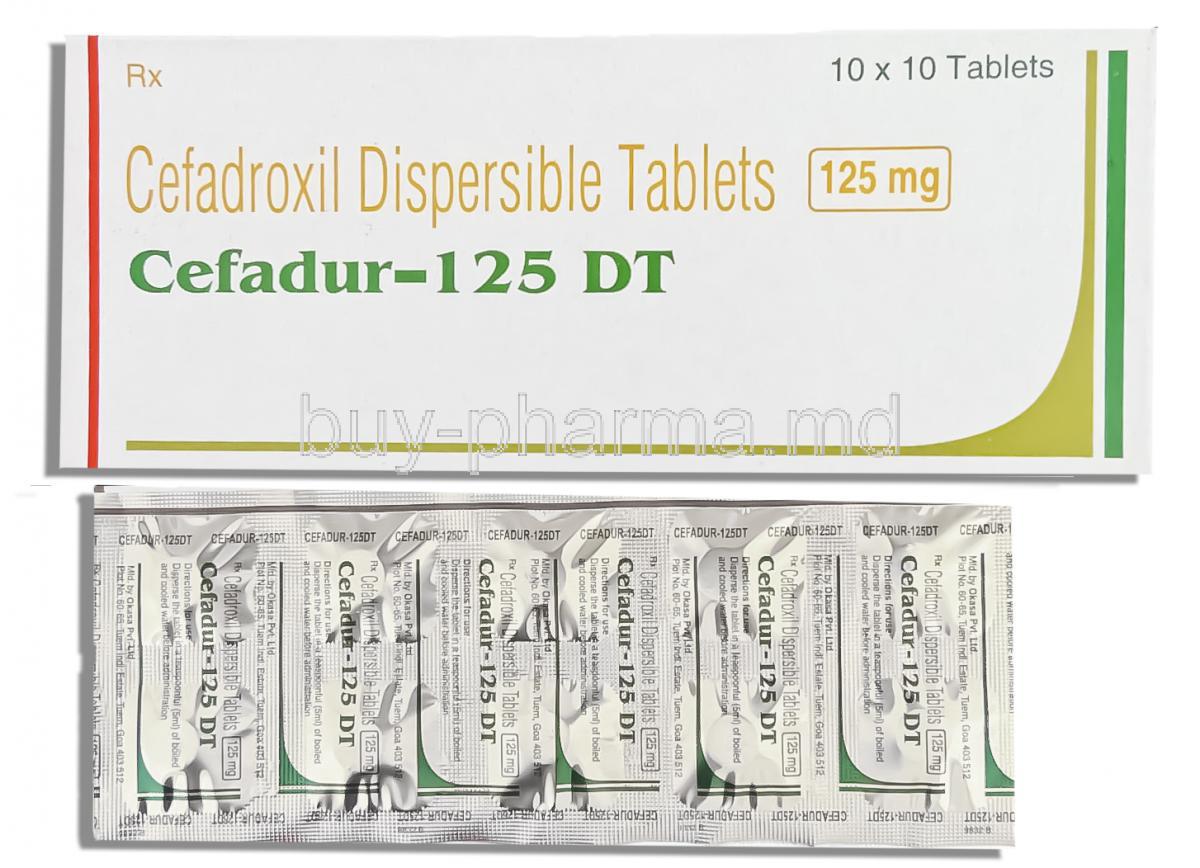
Composition and Formulation
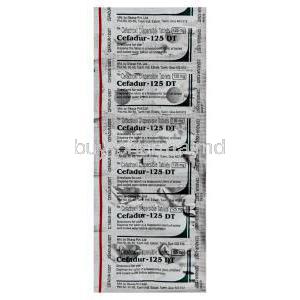
The primary active ingredient in Cefadur tablets is cefadroxil, offered in commonly available strengths such as 250 mg and 500 mg. Inactive components may include excipients like microcrystalline cellulose, magnesium stearate, sodium starch glycolate, and colorants, all contributing to tablet stability and appearance. Tablets are typically film-coated, available in standard oval or capsule shapes, and may be scored for easier dosing. Packaging configurations often come in protective blister strips or bottles designed to preserve product potency and protect against environmental factors.
Mechanism of Action – How Cefadroxil Works
As a member of the beta-lactam antibiotic class, cefadroxil exerts its antibacterial effect by inhibiting bacterial cell wall synthesis. It binds to penicillin-binding proteins within the bacterial cell, disrupting the cross-linking of peptidoglycan chains essential for structural integrity. This disruption leads to cell lysis and death, making cefadroxil a bactericidal rather than bacteriostatic agent. Its antimicrobial spectrum covers a range of gram-positive organisms, such as Streptococcus pyogenes and Staphylococcus aureus, as well as selected gram-negative bacteria like Escherichia coli and Klebsiella pneumoniae.
Approved Medical Uses
- Upper respiratory tract infections – Effective for conditions such as pharyngitis and tonsillitis caused by susceptible bacterial strains.
- Skin and soft tissue infections – Used for cellulitis, impetigo, and other dermal infections requiring systemic antibacterial therapy.
- Urinary tract infections (UTIs) – Indicated for both uncomplicated cystitis and more severe pyelonephritis when caused by sensitive organisms.
- Prevention of recurrent streptococcal infections – Helps reduce the frequency of recurrence in high-risk individuals.
Off-Label and Less Common Uses
- Otitis media – May be prescribed in select cases where other first-line treatments are unsuitable.
- Empiric therapy – Utilized while awaiting culture results in suspected bacterial infections.
- Alternative for certain penicillin-allergic patients – Suitable in individuals without a history of severe anaphylactic reaction to penicillins.
- Dental prophylaxis – Applied in preventing infection in high-risk patients undergoing dental procedures.
Dosage and Administration Guidelines
Typical adult doses range from 500 mg to 1 g every 12 hours, depending on infection type and severity. Pediatric dosing is weight-based, usually between 25–50 mg/kg/day in divided doses. In patients with renal impairment, dosage adjustments are necessary to prevent accumulation. The length of therapy varies, from 5–10 days for mild infections to longer courses for complicated cases. Cefadur may be taken with or without food, though food can help minimize gastrointestinal discomfort. If a dose is missed, it should be taken promptly unless the next scheduled dose is imminent—double dosing is not recommended.
Important Precautions Before Use
Before initiating therapy, a thorough patient history should be obtained to identify any prior allergic reactions to beta-lactam antibiotics. Misuse or incomplete courses may contribute to antibiotic resistance, a growing public health concern. Prolonged use can result in secondary infections, such as Clostridioides difficile-associated diarrhea, which requires immediate medical attention. Vigilance for early signs of hypersensitivity—including rash, swelling, and difficulty breathing—is critical.
Warnings and Safety Alerts
- Severe allergic reactions – Including anaphylaxis and cross-reactivity in penicillin-sensitive individuals.
- Hematologic effects – Rare occurrences of eosinophilia, leukopenia, or neutropenia during therapy.
- Renal monitoring – Recommended for patients receiving prolonged courses, particularly the elderly or those with preexisting kidney conditions.
- Gastrointestinal disease caution – Patients with a history of colitis should use cefadroxil cautiously due to the risk of exacerbation.
Contraindications
- Documented hypersensitivity to cefadroxil, other cephalosporins, or beta-lactam antibiotics.
- History of severe allergic reaction, including anaphylaxis, to penicillin antibiotics.
Careful Administration and Special Monitoring
Patients with renal impairment require careful dosage adjustment to prevent accumulation of cefadroxil, which may lead to toxicity. Regular monitoring of serum creatinine levels and estimated glomerular filtration rate is essential, especially in long-term therapy. For those with hepatic impairment, while primary elimination is renal, the presence of liver disease may influence overall metabolism and necessitate dose modification. Individuals with concurrent conditions such as severe cardiovascular disorders, metabolic diseases, or immune suppression may require tailored regimens to ensure both efficacy and safety.
Administration in Special Populations
Use in Elderly Patients
In elderly individuals, physiological changes—particularly reduced renal clearance—can alter the pharmacokinetics of cefadroxil, leading to higher systemic exposure. This group may be more susceptible to adverse events such as gastrointestinal intolerance or hypersensitivity reactions. Close clinical observation and potential dose reductions are recommended.
Use in Pregnant Women
Cefadroxil is generally classified in a pregnancy safety category indicating that available animal studies have not demonstrated teratogenic effects, though adequate and well-controlled studies in pregnant women are lacking. Prescribing during pregnancy should occur only when the anticipated benefits clearly outweigh potential risks to the fetus, with preference for the lowest effective dose over the shortest possible duration.
Use in Nursing Mothers
Cefadroxil is known to be excreted in human breast milk in low concentrations. While significant adverse effects in nursing infants are rare, gastrointestinal disturbances or allergic reactions may occur. Monitoring the infant for changes in stool pattern, feeding habits, or skin reactions is advisable during maternal therapy.
Use in Children
Pediatric dosing must be carefully calculated based on body weight, commonly ranging from 25–50 mg/kg/day in divided doses. The safety profile in children is generally favorable, with tolerability similar to that in adults. Indications for pediatric use include streptococcal pharyngitis, skin infections, and urinary tract infections caused by susceptible organisms.
Possible Drug Interactions
- Oral anticoagulants (e.g., warfarin) – May potentiate anticoagulant effects, necessitating closer monitoring of prothrombin time or INR.
- Bacteriostatic antibiotics such as tetracyclines – May reduce the bactericidal efficacy of cefadroxil by antagonistic action.
- Laboratory test interference – May cause false-positive results in certain glucose urine tests; enzymatic methods should be used for accuracy.
Side Effects of Cefadur (Cefadroxil)
Common Side Effects
- Diarrhea, nausea, and vomiting
- Abdominal discomfort or indigestion
- Mild skin rash and itching (pruritus)
Serious and Rare Side Effects
- Anaphylaxis and other severe hypersensitivity reactions requiring immediate medical attention
- Severe cutaneous reactions such as Stevens–Johnson syndrome and toxic epidermal necrolysis
- Clostridioides difficile-associated diarrhea, potentially life-threatening
- Hematologic abnormalities including thrombocytopenia and leukopenia
Overdose Management
Signs of overdose may include pronounced gastrointestinal distress such as severe nausea, vomiting, and diarrhea, as well as rare neurologic manifestations like seizures. Management is primarily supportive, focusing on hydration, electrolyte balance, and symptomatic relief. In cases of severe overdose, hemodialysis can aid in drug removal from circulation, particularly in patients with renal compromise.
Handling and Storage Guidelines
- Store at controlled room temperature, ideally between 20°C and 25°C, away from excess moisture and direct light.
- Maintain in original packaging until use to ensure stability and prevent contamination.
- Keep out of reach of children and pets to avoid accidental ingestion.
- Dispose of unused or expired medication responsibly, following local pharmaceutical disposal regulations.
Handling Precautions for Healthcare Providers
When dispensing cefadroxil, healthcare professionals should adhere to proper infection control measures. Avoid direct skin contact with powdered or crushed tablets to minimize exposure risk. Work surfaces should be clean and dry, and protective equipment may be used when preparing doses in clinical settings. These precautions help maintain both patient safety and medication integrity.
Cefadur, Cefadroxil Tablet FAQ
- What are cefadroxil tablets used for?
- When is the best time to take cefadroxil?
- Is cefadroxil effective for UTI?
- What is the warning for cefadroxil?
- Is cefadroxil a strong antibiotic?
- What are the side effects of cefadroxil 500 mg?
- How to know if cefadroxil is working?
- How long does cefadroxil stay in your system?
- When to stop taking cefadroxil?
- What not to take with cefadroxil?
- Are cefalexin and cefadroxil the same?
- Will cefadroxil make you tired?
- What is another name for cefadroxil?
- Is cefadroxil better than azithromycin?
- What is cefadroxil best for?
- Do you need a prescription for cefadroxil?
- Does cefadroxil cause weight gain?
- What is the warning for cefadroxil?
- How strong is cefadroxil?
- Is cefadroxil discontinued?
- Is cefadroxil a antibiotic tablet?
- How many days should you take cefadroxil 500mg?
- Is cefadroxil a safe antibiotic?
What are cefadroxil tablets used for?
Cefadroxil is basically a type of antibiotic that helps fight off infections in parts of the body. It's part of a group of medicines called cephalosporins.
When is the best time to take cefadroxil?
With or without food every 12 or 24 hours
Is cefadroxil effective for UTI?
Yes
What is the warning for cefadroxil?
This medicine may cause serious skin reactions
Is cefadroxil a strong antibiotic?
Yes
What are the side effects of cefadroxil 500 mg?
Rash and Diarrhea
How to know if cefadroxil is working?
You should start to feel better within the first few days.
How long does cefadroxil stay in your system?
24 hours
When to stop taking cefadroxil?
7 days or until the prescription stops.
What not to take with cefadroxil?
Benzydamine, Benzyl alcohol, Abacavir, Abciximab, Acemetacin
Are cefalexin and cefadroxil the same?
Cefadroxil is excreted from the body more slowly than cephalexin. This allows less of the medicine.
Will cefadroxil make you tired?
Yes
What is another name for cefadroxil?
Cefadur
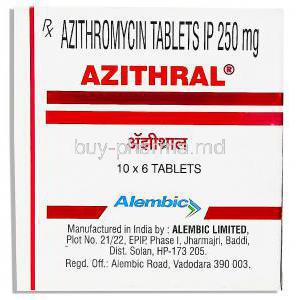
Is cefadroxil better than azithromycin?
Yes
What is cefadroxil best for?
Cefadroxil is an antibiotic that's effective against a range of infections. It's part of a group of medicines called cephalosporins. It works by either killing off the bacteria or stopping them from growing in the place.
Do you need a prescription for cefadroxil?
Yes
Does cefadroxil cause weight gain?
Yes
What is the warning for cefadroxil?
This medicine may cause serious skin reactions.
How strong is cefadroxil?
Cefadroxil is an antibiotic that's really effective against a range of bacterial infections.
Is cefadroxil discontinued?
No
Is cefadroxil a antibiotic tablet?
Yes
How many days should you take cefadroxil 500mg?
10 days
Is cefadroxil a safe antibiotic?
Some people can have a reaction to Cefadroxil.