Clincin, Clindamycin
- Introduction to Clindamycin (Clincin)
- Composition of Clindamycin
- How Clindamycin Works
- Uses of Clindamycin
- Off-Label Uses of Clindamycin
- Dosage and Administration of Clindamycin
- Side Effects of Clindamycin
- Common Side Effects of Clindamycin
- Important Precautions with Clindamycin
- Interactions of Clindamycin with Other Medications
- Warnings and Contraindications
- Careful Administration of Clindamycin
- Administration to Special Populations
- Overdose and Emergency Management
- Storage and Handling Precautions for Clindamycin
- Conclusion
Introduction to Clindamycin (Clincin)
Clindamycin, known as Clincin in the market is a component of today's antimicrobial treatments. This antibiotic stands out for its effectiveness and wide range of impact contributing significantly to the fight against infections. The evolution of Clindamycin from its beginnings to its status as a key player in medicine is attributed to innovative research and progress. Its significance, in healthcare, is immense offering healthcare providers a powerful tool to combat various harmful bacteria.
Overview of Clindamycin
Clindamycin stands as an example of how antibiotic treatment has progressed over time. It emerged in the 1960s from a soil bacterium called Streptomyces lincolnensis marking a milestone in the field of pharmaceutical science. The creation of this drug was spurred by the pressing demand for antibiotics that could effectively tackle stubborn bacterial strains. Presently Clindamycin continues to play a role, in multiple areas of medicine highlighting its flexibility and crucial role in combating bacterial infections.
Historical Background and Development
Clindamycin origins can be linked to a time when bacteria were becoming resistant, to antibiotics. Scientists seeking answers discovered the promise of Clindamycin. Its creation was not a stroke of luck but the outcome of careful research focused on improving the way existing antibiotics work in the body. The result of these efforts was an antibiotic that not only widened its ability to fight microbes but also had favorable characteristics when it came to being absorbed and distributed in the body.
Importance in Modern Medicine
- Clindamycin plays a role in combating anaerobic bacteria and specific parasites highlighting its importance in treatment strategies.
- Its effectiveness in addressing infections affecting the skin respiratory system and bones demonstrates its versatility.
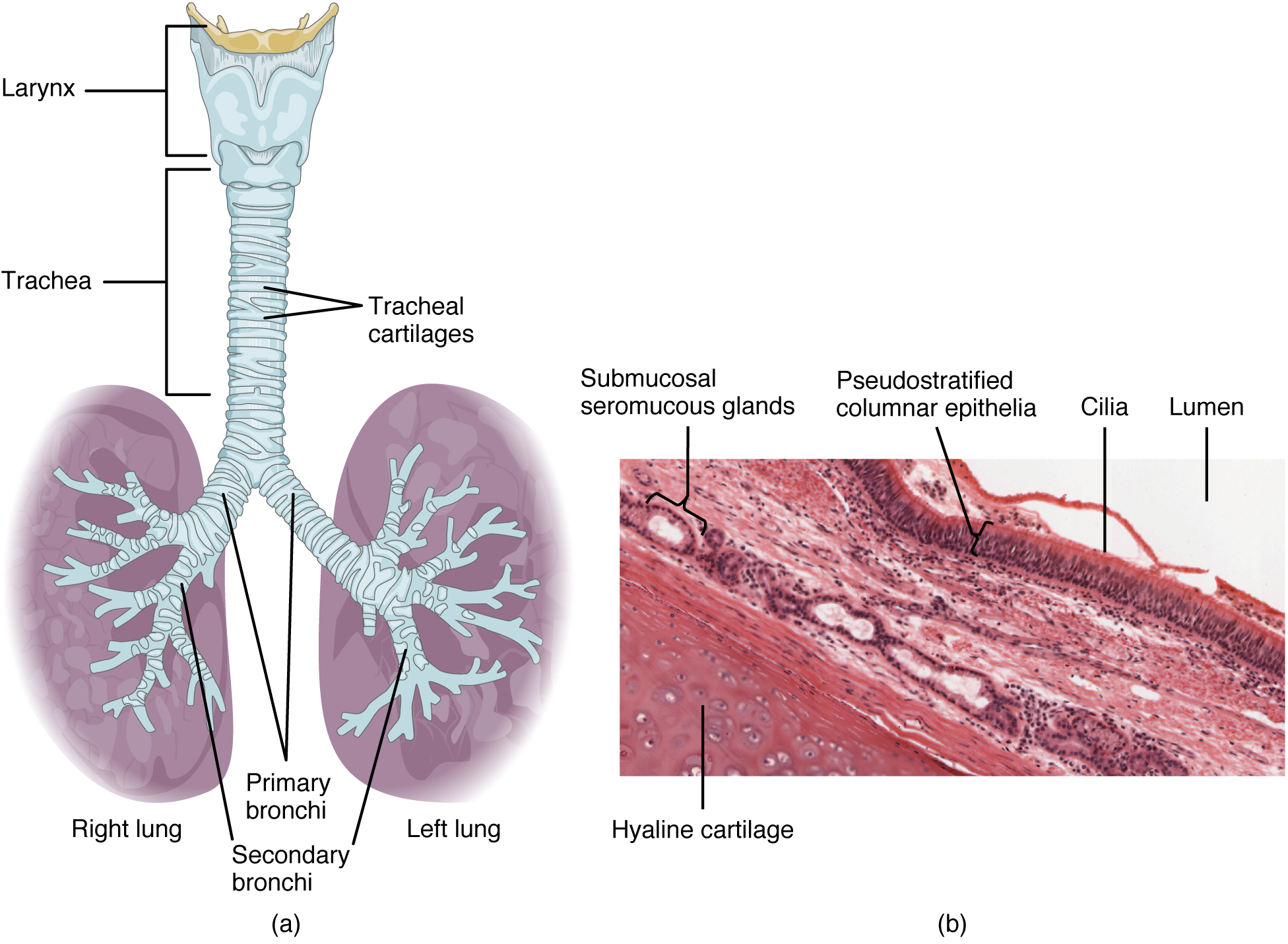
Respiratory-System
- The medication is highly valued for its capability to reach bone tissue, which is essential, for managing osteomyelitis.
Composition of Clindamycin
Clindamycin is made up of a combination of its main active component and additional substances each with its own specific role. The effectiveness of Clindamycin lies in its ingredient, which works to prevent the growth of bacteria by blocking protein production in susceptible strains.
This is complemented by forms such as capsules, injections, and topical treatments designed to cater to various medical requirements. Although the inactive ingredients have no pharmacological effects they are vital for maintaining the antibiotic's stability, and absorption, into the body and taste.
Active Ingredient Analysis
The main component, which is Clindamycin phosphate is a form of the original substance Clindamycin. This modification improves how well the drug dissolves in water. Makes it easier to include different types of medications. The clever design of the ingredient, in Clindamycin showcases advancements in pharmaceuticals making sure it works effectively for treatment and is easy for patients to use.
Formulations Available: Capsules, Injectable, Topical
- Capsules are a choice for easily taking medication orally to treat various infections.
- Injectable options are typically used for infections to quickly deliver the medication into the bloodstream.
- Topical treatments like creams and gels are applied directly on the skin to address issues, like acne and other skin infections.

Cream Application
Inactive Ingredients and Their Roles
The nonactive elements found in Clindamycin products consist of substances that help maintain the drug stability prevent the growth of microorganisms and improve the consistency of forms. Including these ingredients showcases the precision involved in pharmaceutical production guaranteeing that the end result is both efficient and easy to use.
How Clindamycin Works
Clindamycin's way of working is quite complex and intriguing. It attaches to the 50S part of the ribosome blocking the initial steps of creating proteins. This method makes it stops bacteria growth acting as a barrier against bacteria. With its spectrum of effectiveness, this antibiotic can combat various pathogens such as anaerobic and certain aerobic bacteria. Its versatility in targeting an array of bacteria distinguishes it from other antibiotics making it a valuable asset, for healthcare professionals.
Mechanism of Action Against Bacteria
The beauty of how Clindamycin works is in its precision. It focuses on the ribosome while leaving human cells untouched reducing the risk of side effects. This focused method, combined with its ability to reach into tissues enables Clindamycin to fight infections, in hard-to-reach areas effectively.
Spectrum of Antimicrobial Activity
Clindamycin is effective against a variety of bacteria that are resistant to other antibiotics. Its ability to combat MRSA and the anaerobes that cause dental infections showcases its role, in modern antimicrobial treatment.
Comparison with Other Antibiotics
When compared to antibiotics Clindamycin stands out for its distinct characteristics. Its capability to reach bone tissue and effectiveness against a range of bacteria sets it apart from many other antibiotics. Additionally, its flexibility in formulation allows for customized treatment approaches enhancing its usefulness, in medical situations.
Uses of Clindamycin
Clindamycin(1), a component of antimicrobial treatments is widely utilized for fighting various bacterial infections.(2) It plays a role not just in curing infections but also in preventing them during surgical procedures(3) illustrating its diverse uses in the field of clinical medicine. Its effectiveness in treating infections across body areas from skin to bone deep within the body highlights its vital importance, in the healthcare sector.
1. NCBI - Clindamycin
2. Medline - Clindamycin
Indications in Bacterial Infections
Clindamycin is highly effective in treating bacterial infections caused by vulnerable strains(1). It is an antibiotic for combating anaerobic bacteria and specific aerobic organisms playing a crucial role in the medical fight, against bacterial pathogens.
1. National Library of Medicine -Current indications for the use of clindamycin: A critical review
Skin and Soft Tissue Infections
Clindamycin is highly effective in treating infections on the skin and soft tissues caused by Staphylococcus aureus and Streptococcus pyogenes(1). Its capability to reach layers of the skin enables it to combat serious conditions, like cellulitis and abscesses effectively.
1. Science Direct - Clindamycin
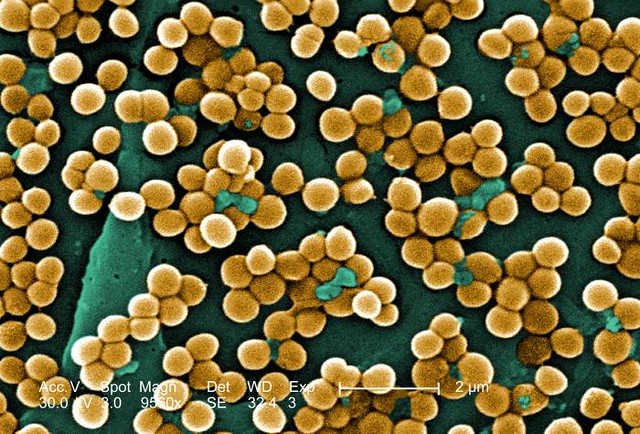
Staphylococcus-aureus under the microscope
Respiratory Tract Infections
The antibiotic works well in treating tract infections especially those caused by anaerobic bacteria.(1) Clindamycin is commonly used to treat pneumonia, bronchitis, and lung abscesses offering relief by eliminating the causes.
1. Science Direct - Clindamycin
Bone and Joint Infections
Clindamycin's ability to deeply penetrate bone tissue makes it a powerful remedy for osteomyelitis and septic arthritis. This quality is especially advantageous considering the difficulty, in delivering drug levels to sites of bone infection.
Intra-abdominal Infections
In the field of infections within the abdomen, Clindamycin has shown effectiveness in combating the bacteria that cause peritonitis and abscesses in the region. Its ability to target bacteria is particularly important, in these situations as these types of pathogens are most common.
Gynecological Infections
Clindamycin is useful for addressing infections in the reproductive system, such as bacterial vaginosis, endometritis, and pelvic inflammatory disease. Its efficacy, in these situations, highlights its significance in promoting women health.
Role in Surgical Prophylaxis
The use of Clindamycin as a measure in surgical procedures is well documented. It is utilized to prevent infections at the site, especially in situations where allergies to penicillin make it impossible to use beta-lactam antibiotics. This proactive approach highlights the spectrum effectiveness of the antibiotic and its ability to stop infections before they start.
To sum up, Clindamycin's wide range of uses in treating bacterial infections along with its role in preventing infections during surgery solidifies its position as a key player in antimicrobial treatment. The drug's versatility and effectiveness across conditions underline its importance, in modern medicine.
Off-Label Uses of Clindamycin
Clindamycin, an antibiotic offers more than just its intended uses. Its use in dermatology combating bacteria and in treating children showcase how effective and versatile this medication can be in response, to changing medical requirements. By using it healthcare providers can leverage Clindamycins capabilities to treat a range of conditions that may not have been originally specified in its approval.
Treatment of Acne and Other Dermatological Conditions
Clindamycin's application in dermatology for addressing acne concerns highlights its effectiveness in managing skin issues. Its antibacterial properties along with its inflammatory capabilities make it a popular choice for treating acne vulgaris. Additionally, it is utilized in the treatment of other skin conditions where bacterial infections are significant providing relief and enhancing patient outcomes. Its ability to reduce acne lesions through its anti-inflammatory and antibacterial actions is well recognized. It is also versatile in treating skin infections, like folliculitis and impetigo.
Use in Combating Methicillin-resistant Staphylococcus aureus (MRSA)
One of the interesting unconventional uses of Clindamycin is its effectiveness against MRSA, a strong pathogen that resists many traditional antibiotics. When dealing with suspected or confirmed cases of MRSA Clindamycin provides an alternative, especially in situations where other treatments have been ineffective or cannot be tolerated. This demonstrates the role Clindamycin plays in treating infections during a time when antibiotic resistance is on the rise. It is an option in fighting against MRSA, particularly for skin and soft tissue infections. Its use in treating MRSA infections highlights the necessity, for antibiotic approaches when facing resistant pathogens.
Application in Pediatric Infections Beyond Label Indications
The use of Clindamycin in children for purposes not specified on its label demonstrates its ranging effectiveness and safety. Its ability to treat serious infections like osteomyelitis, septic arthritis, and abdominal abscesses in pediatric patients shows how valuable this drug is in pediatric healthcare.
Clindamycin plays a role in managing complex infections in children, where having safe and reliable treatment options is essential.
Its off-label use highlights the importance of tailoring treatment plans to meet each child's needs and medical conditions. In essence, the diverse applications of Clindamycin beyond its approved uses signify the evolving landscape of medical care.
From addressing skin conditions to combating antibiotic bacteria such as MRSA and treating infections in children Clindamycin proves to be a versatile and indispensable antibiotic in modern medicine. These varied uses emphasize the need, for innovative treatment strategies to effectively tackle the challenges posed by bacterial infections.
Dosage and Administration of Clindamycin
Clindamycin is a weapon, in fighting bacterial infections, its dosage and how its given are customized to maximize its healing benefits and reduce side effects. It's crucial to dose precisely based on the patients needs and condition for the best results.
Dosage Guidelines for Different Conditions
The amount of Clindamycin needed can vary based on the type and seriousness of the infection it is used to treat. Typically adults take between 150 to 450 mg orally every 6 to 8 hours while intravenous doses can range from 600 to 900 mg every 8 hours depending on how severe the infection is.
Lower doses are usually enough for skin and soft tissue infections. For more serious infections, like intra-abdominal abscesses higher doses are often required.
Route-specific Administration: Oral, Intravenous, Topical
The method of giving Clindamycin depends on where the infection how serious it is, along with the patient's condition. Typically oral intake is used for mild infections while intravenous administration is preferred for more severe cases and topical application is commonly used for localized skin infections.
- Oral forms like capsules and liquids are convenient for outpatient treatment. Intravenous delivery ensures the distribution of the medication in severe infection scenarios.
- Topical formulations like creams and lotions are directly applied to the skin areas, for skin infections.
Adjustments for Renal and Hepatic Impairment
It's important to make changes in the dosage of Clindamycin for patients with issues in their liver or kidneys. While Clindamycin mostly gets broken down in the liver it's still important to be cautious in both situations to prevent buildup and a higher chance of effects
. When it comes to liver problems adjusting the dose or keeping an eye on things might be needed. As, for kidney issues usually the Clindamycin dose doesn't need changing. It's good to monitor patients more closely.
Side Effects of Clindamycin
The effectiveness of Clindamycin for therapy although significant comes with a variety of side effects spanning from minor to severe. Being aware of and promptly addressing these outcomes is essential, for providing the best care to patients.
Overview of Common and Serious Side Effects
The side effects of clindamycin can include gastrointestinal, skin-related and overall body reactions. Although most patients can handle the medication without issues it's crucial to stay alert, for any signs of serious complications.
Gastrointestinal Disturbances: Risk of Clostridium difficile-associated Diarrhea
The use of Clindamycin carries a risk of causing Clostridium difficile-associated diarrhea (CDAD) which can manifest as anything, from minor diarrhea to severe colitis. Clindamycin disrupts the balance of gut bacteria leading to the growth of C. Difficile highlighting the importance of closely monitoring gastrointestinal symptoms.
Allergic Reactions and Hypersensitivity
Less frequent but still possible allergic responses to Clindamycin may appear as skin irritations, hives, or, in some situations, anaphylaxis. It is crucial to seek medical help upon noticing any indications of hypersensitivity.
Liver Enzyme Abnormalities
Temporary rises in liver enzyme levels can happen when using Clindamycin so it's important to keep an eye on liver function for patients, on treatment.
Common Side Effects of Clindamycin
The range of side effects associated with Clindamycin is extensive but some negative reactions are more commonly seen in actual medical practice.
Skin Rash, Itching, Hives
Skin reactions such, as rashes, itching, and hives are frequently observed as side effects often suggesting mild allergic reactions.
Nausea, Vomiting, Diarrhea
Patients commonly experience issues, like queasiness throwing up, and loose stools, which can usually be controlled with proper care and drinking enough fluids.
Oral Thrush or Vaginal Yeast Infection
Disrupting the balance of bacteria in our bodies can result in opportunistic infections such as oral thrush or vaginal yeast infections, which may call for antifungal medication in addition to Clindamycin treatment. To sum up, it's clear that Clindamycin plays a role in combating bacterial infections but its usage demands a detailed understanding of dosage plans and close monitoring for potential side effects. By managing patients, with care and attention, we can harness the benefits of Clindamycin to ensure effective treatment outcomes while minimizing the chances of negative impacts.
Important Precautions with Clindamycin
Clindamycin, an antibiotic should be used carefully with an understanding of its precautions to ensure patient safety and improve treatment effectiveness.
Avoidance in Individuals with a History of Colitis
One important safety measure is to avoid using Clindamycin in people who have had colitis before antibiotic-related colitis. This careful approach is due, to the fact that Clindamycin has the ability to disrupt the balance of gut bacteria, which can lead to the development or worsening of colitis.
Monitoring for Signs of Anaphylaxis
Although the possibility of anaphylaxis, an allergic reaction that can be life-threatening requires careful observation after administering Clindamycin. Healthcare providers should be ready to take action if symptoms of anaphylaxis appear.
Importance of Completing the Full Course of Therapy
Making sure that patients finish the Clindamycin treatment is really important to get rid of the infection completely and stop antibiotic resistance from happening. Stopping the treatment soon could not only affect the recovery process but also lead to the growth of bacteria that are resistant, to antibiotics.
Interactions of Clindamycin with Other Medications
The effectiveness and safety characteristics of Clindamycin might change based on how it interacts with drugs. It's crucial for healthcare providers to be aware of these interactions to prevent effects and provide the best care, for patients.
Potential for Antagonism with Certain Antibiotics
Clindamycin might not work well when taken with antibiotics like erythromycin. This could reduce the effectiveness of the treatment underscoring the need, for medication review before starting Clindamycin therapy.
Effects on the Efficacy of Oral Contraceptives
While the evidence is varied there is a worry that antibiotics, like Clindamycin, might lower the effectiveness of birth control pills. It is recommended that patients think about using contraceptive methods while undergoing Clindamycin treatment.
Interaction with Neuromuscular Blocking Agents
In settings, it has been noted that Clindamycin can enhance the impact of neuromuscular blocking agents potentially prolonging the period of neuromuscular blockade under anesthesia. Due to this interaction, careful monitoring is required to make adjustments, to the anesthesia.
Warnings and Contraindications
The use of clindamycin comes with cautions and restrictions designed to reduce possible harm to patients. It is crucial for healthcare professionals to follow these guidelines to maintain safety.
Contraindications for Use in Patients with Certain Conditions
Clindamycin should not be used in individuals who have shown sensitivity to the medication or its ingredients. It is also important to be cautious when prescribing it to patients with a history of issues especially those prone, to colitis as it may worsen these conditions.
Warning Regarding the Use in Patients with a History of Gastrointestinal Disease
Patients who have previously had issues, particularly those related to the colon should be carefully evaluated before starting Clindamycin treatment. The risk of Clindamycin causing colitis highlights the importance of thoroughly assessing the balance between risks and benefits in these individuals.
In essence although Clindamycin is an antibiotic, for treating various bacterial infections it comes with significant precautions, potential interactions, warnings, and contraindications. It is crucial to follow these guidelines to ensure optimal treatment outcomes while protecting well-being.
Careful Administration of Clindamycin
When it comes to using clindamycin, an adaptable antibiotic it's crucial to be very careful especially when dealing with people who are more susceptible to its impact. It's essential to take care of elderly individuals and those, with liver or kidney issues to create treatment strategies that work effectively while reducing any potential risks.
Special Considerations for Elderly Patients
Older individuals might experience increased sensitivity to Clindamycin requiring dosage adjustments to reduce the chances of reactions. Changes in how the body processes drugs due to aging like reduced kidney function and shifts, in drug distribution highlight the importance of being careful when administering medications.
Dosing Considerations in Patients with Liver or Kidney Disease
Patients who have liver or kidney issues pose a consideration when it comes to administering Clindamycin. It is important to monitor them and potentially adjust the dosage to prevent any build-up of the drug leading to toxicity. In instances of liver problems, healthcare providers need to assess the level of impairment and modify the dosing as necessary. Even though Clindamycin is mainly metabolized in the liver caution is recommended for individuals with kidney disease due to changes, in drug elimination.
Administration to Special Populations
When giving Clindamycin to groups like pregnant women breastfeeding mothers, children, and older individuals it's important to have a detailed understanding of how the drug works and its effects, on these vulnerable populations.
Guidelines for Pregnant Women and Nursing Mothers
During pregnancy, it is recommended to use Clindamycin only if the advantages are greater than the risks as research on animals has indicated negative impacts, on the growth of fetuses. For breastfeeding mothers, it's important to be careful since the medication can enter breast milk and potentially impact the baby.

Pregnant Woman
Pediatric Administration: Safety and Efficacy
When prescribing Clindamycin to children it is crucial to strike a balance, between effectiveness and safety. Although it is widely deemed safe the dosage should be adjusted according to the child's weight and the seriousness of the infection in order to reduce the chances of negative reactions.
Considerations for Elderly Patients: Dosing and Side Effects
Elderly individuals need personalized dosage plans to address changes in their bodies that impact how medications are processed and eliminated. Understanding the likelihood of experiencing side effects like stomach problems and the risk of severe colitis is vital, for this age group.
Overdose and Emergency Management
Overdosing on Clindamycin though uncommon can happen, requiring identification and intervention to minimize negative effects. It is crucial for healthcare professionals to recognize the indications, manifestations, and available treatment choices.
Signs and Symptoms of Clindamycin Overdose
Symptoms of taking too much Clindamycin can manifest as severe stomach issues like feeling sick throwing up and having diarrhea along, with potential neurological signs. It is crucial to recognize these indicators to ensure proper treatment.
Immediate Steps and Supportive Care
In case of an overdose, the first priority is to provide care by ensuring proper airway, breathing, and circulation. Consideration may be given to decontamination based on the timing and amount of the overdose.
Antidote and Treatment Options
There isn't an antidote for an overdose of Clindamycin so treatment mainly involves providing support. This may include giving fluids through an IV for hydration balancing electrolytes and keeping an eye out for signs of reactions like anaphylaxis. To sum up, when administering Clindamycin to certain groups and in cases of overdose it's important to have a full grasp of how it moves through the body and the potential negative effects. By evaluating patients and keeping a close watch, on them, healthcare professionals can maximize the positive effects of Clindamycin while reducing the risks that come with its use.
Storage and Handling Precautions for Clindamycin
Making sure that Clindamycin works well and is safe depends on following the storage and handling procedures. These protocols help protect the quality of the medication ensuring that it can deliver its healing benefits to patients when used.
Recommended Storage Conditions
Store clindamycin at room temperature keeping it away from light and moisture to keep it effective. Both oral and topical versions should be stored in a dry place ideally, between 20°C to 25°C (68°F to 77°F) with slight variations allowed between 15°C to 30°C (59°F to 86°F).
Shelf Life and Disposal of Expired Medication
The duration for which Clindamycin remains differs depending on the form it comes in usually lasting between two to three years from the manufacturing date when stored correctly. When it reaches its expiration date it's important to discard the medication following guidelines to avoid harming the environment or accidental consumption.
It is not recommended to flush expired medications down the toilet or simply throw them in household trash; instead consider utilizing take-back programs provided by pharmacies and local health departments for disposal of unused or expired medications.
Handling Precautions for Healthcare Providers
When working with Clindamycin in its injectable form healthcare professionals need to take standard precautions to prevent accidental exposure through skin contact or inhalation. It's important to use gear like gloves and masks when preparing and administering the medication to reduce the chances of any negative effects.
Conclusion
The use of Clindamycin, known for its range of antibacterial effects is crucial in modern healthcare. Its effectiveness, in combating bacterial infections highlights the significance of this antibiotic in fighting against harmful microbes.
Summary of Key Points About Clindamycin
Clindamycin plays a role in the field of medicine providing vital support, in treating severe bacterial infections. It is important to store and handle it correctly follow dosage instructions diligently and be mindful of side effects and drug interactions to fully leverage its healing properties.
The Role of Clindamycin in Current Medical Practice
In today's field, Clindamycin is still considered a crucial medication for managing infections that show resistance to other antibiotics. It serves not as a treatment option but also plays a vital role in preventative measures during surgeries and dealing with complicated infections, in specific groups of people.
Future Outlook and Ongoing Research
The future of Clindamycin relies heavily on research efforts to improve its effectiveness minimize side effects and tackle resistance issues. Current studies investigating forms and combined treatments show promise in expanding its use against bacterial infections ensuring Clindamycin remains a crucial part of global health strategies. Overall clindamycin's versatile role in treatment, which depends on proper storage, handling, and administration procedures showcases its lasting importance in addressing the challenges presented by bacterial infections. As research advances its place in care is set to develop further reinforcing its position, as an essential antibiotic.