Introduction to Endace (Megestrol Acetate Tablet)
Overview of megestrol acetate as a synthetic progestational agent
Megestrol acetate is a potent synthetic derivative of the naturally occurring hormone progesterone. It manifests a multifaceted pharmacodynamic profile. Some individuals utilize it to help counter catabolic weight loss, while others benefit from its cytostatic effect in certain hormone-responsive neoplasms. • Structural similarity to endogenous progesterone • Ability to exert strong progestogenic receptor binding
Therapeutic class and pharmacologic category
This medication is categorized primarily within the progestational hormone modulators. In clinical usage, it is recognized as both an appetite stimulant and antineoplastic support therapy. Its classification aligns with hormonal oncology-supportive strategies.
Brief mention of approved indications and evolving clinical roles
Approved regulatory indications include anorexia with cachexia in chronic disease and adjunctive therapeutic support in hormone-responsive malignancies. As clinical evidence evolves, its therapeutic applicability continues to expand across metabolic and endocrine-adjacent areas.
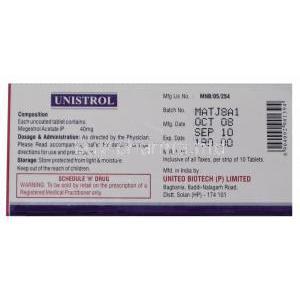
Composition and Formulation Details
Active ingredient and strength variations of Megestrol Acetate Tablet
The core pharmacologic entity is Megestrol Acetate in standardized tablet strengths. These strengths may be calibrated depending on clinical intent or disease burden.
Excipients and tablet formulation characteristics
The tablets incorporate stability excipients, compression binders, and disintegration facilitators. • Controlled disintegration profile • Ensured systemic bioavailability after ingestion
Oral dosage form and pharmacotechnical properties
Oral tablets are engineered to yield reproducible plasma concentration curves. Sustained exposure often translates to extended appetite enhancement and anti-neoplastic receptor modulation.
How Endace Works – Mechanism of Action Explained
Progestational receptor activity and endocrine effects
Megestrol acetate binds to progesterone receptors in endocrine-relevant tissues. This perturbs hypothalamic-pituitary axis signals and alters cellular transcriptional behavior. The resulting cascade exhibits both therapeutic and metabolic influence.
Appetite-stimulation pathways and metabolic influence
This agent modulates appetite-governing neurochemistry. • Enhancement of hunger signaling • Shift in anabolic substrate utilization • Incremental caloric intake facilitation
Immunologic modulation effects related to anti-neoplastic activity
Antiproliferative and immune-modulatory impacts can attenuate tumor progression in sensitive malignancies. Cellular cytokine expression may be altered, resulting in a favorable antitumor milieu in some settings.
Primary Uses of Endace (Approved Indications)
Management of anorexia, cachexia, or significant weight loss in chronic illness
Endace is widely applied in disease-associated weight loss states. Cancer and chronic illness patients often experience hypercatabolic stress, and megestrol acetate helps restore weight trajectory.
Adjunct treatment in advanced breast cancer
Hormone-responsive breast cancer in advanced phases can benefit from progestational blockade of malignant cell propagation.
Adjunct treatment in advanced endometrial carcinoma
In advanced endometrial carcinoma cases, this agent may act to reduce tumor volume and mitigate symptom progression.
Off-Label Uses of Megestrol Acetate
Appetite improvement in AIDS-related wasting syndrome
Many clinicians utilize it in HIV-related cachexia.
Appetite support in geriatric weight loss and frailty
Selected elderly populations demonstrate measurable benefit in weight repletion.
Weight gain support in oncology-related cachexia
Tumor-associated metabolic burden is often counteracted with this therapy.
Hormonal therapy considerations in transgender care (female-to-male blockers reversed perspective)
Some endocrinology specialists have adopted selective dosing for hormonal axis modulation strategies.
Adjunctive role in refractory hot flashes not responding to standard management
In rare vasomotor dysregulation, this medicine may impart thermoregulatory stabilization.
Dosage and Administration Guidelines
General recommended dosing ranges for each indication
Dosage ranges differ dramatically between oncologic and appetite-support use cases. • Higher dosing in malignancy • Tailored lower dosing in metabolic wasting syndromes
Titration and dose adjustments based on clinical response
Titration is often prudent due to metabolic sensitivity variances.
Administration schedule, with/without food considerations
Tablets may be ingested with or without meals. Clinicians frequently tie administration to daytime hours for hunger enhancement.
Duration of treatment and discontinuation strategy
Treatment tenure varies. Gradual tapering may be recommended to prevent adrenal withdrawal-like syndromes.
Side Effects Overview
Summary of adverse effect profile by system category
The adverse event spectrum spans metabolic, endocrine, hematologic, and cardiovascular domains. Many reactions stem from glucocorticoid-like receptor cross-stimulation.
Endocrine, metabolic, and cardiovascular impact
• Hyperglycemia • Dyslipidemia • Increased thrombotic risk These perturbations necessitate vigilant monitoring.
Risk of adrenal suppression and glucocorticoid-like effects
Chronic administration may subdue adrenal corticosteroid output, thereby requiring cautious taper when discontinuing.
Common Side Effects Patients May Experience
Weight gain, increased appetite
A hallmark desired outcome yet regarded as an adverse effect in weight-neutral populations.
Edema and fluid retention
Fluid shifts result from endocrine receptor stimulation.
Hyperglycemia and worsening diabetes control
Insulin-resistant states often worsen.
Thromboembolism risk
Immobilized or predisposed individuals may experience heightened clot formation.
Mood changes and sleep disturbances
Altered neurochemical tone may yield insomnia or emotional lability.
Drug Interactions with Endace
Interaction with corticosteroids and related endocrine agents
Synergistic glucocorticoid effects may amplify metabolic toxicity.
Interaction with antidiabetic therapies due to glycemic changes
Adjusting insulin or oral antidiabetic dosing may become necessary.
Interaction with anticoagulants and increased thrombosis potential
Co-administration requires strict clinical vigilance.
CYP metabolism considerations and co-administered therapies
Metabolic processing through hepatic enzymatic pathways may generate cumulative plasma concentration fluctuations.
Important Warnings and Precautions
Thromboembolic event risk and vascular monitoring
Clinicians should evaluate venous circulation status routinely in susceptible cohorts.
Adrenal suppression, tapering recommendations, stress-dose steroid considerations
Perioperative and stress-state steroid supplementation may be mandatory.
Hyperglycemia monitoring in high-risk patients
Glucose monitoring is imperative in diabetogenic risk groups.
Fluid retention and cardiovascular strain in CHF patients
Congestive heart failure may be exacerbated by fluid retention and requires calibrated dosing oversight. ```html
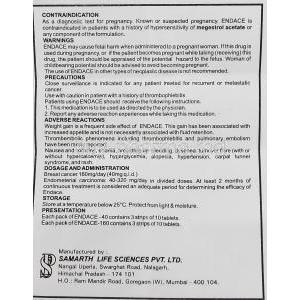
Contraindications for Megestrol Acetate
Active thromboembolic disorders
Megestrol acetate is contraindicated in individuals with existing venous or arterial thromboembolism. Hypercoagulability may be worsened, which can precipitate catastrophic vascular events such as pulmonary embolus or deep venous thrombosis. • Elevated coagulant risk • Detrimental vascular propagation potential
Known hypersensitivity to megestrol acetate
Any prior anaphylactoid or delayed hypersensitivity reaction to this compound precludes re-exposure. The risk of systemic inflammatory flare or dermal eruption is clinically unacceptable in such cases.
Pregnancy-related contraindications
Megestrol acetate must not be administered during pregnancy. Its hormonal modulation may interfere with fetal endocrine pathways, and the embryogenic risk is significant.
Uncontrolled diabetes with complications
In poorly controlled diabetic states, this therapy may escalate glycemic dysregulation. • Exacerbated insulin resistance • Higher probability of severe metabolic decompensation
Careful Administration and Special Considerations
Patients with history of cardiovascular disease
Cardiovascularly vulnerable individuals may experience augmented hemodynamic strain, particularly if fluid retention develops.
Those with long-standing diabetes mellitus
Close glucose surveillance is imperative. Glycemic destabilization may manifest quickly.
Patients with liver impairment
Reduced hepatic clearance may enhance systemic exposure. Consider conservative titration and continual hepatic function review.
Those with chronic kidney disease
Electrolyte disturbances linked to altered renal physiology may be magnified when using this agent.
Administration to Elderly Patients
Frailty considerations and risk-benefit assessment
Older populations frequently present sarcopenia and physiologic reserve reduction. Benefit must clearly outweigh thrombotic and metabolic risk.
Dose minimization and slow titration strategies
• Start at the lower end of the therapeutic spectrum • Increment using small titration increments
Monitoring for thromboembolism in sedentary individuals
Sedentary status exponentially increases clotting risk. Lower limb edema, dyspnea, and new chest discomfort warrant urgent evaluation.
Administration to Pregnant Women and Nursing Mothers
Pregnancy risk categorization
Megestrol acetate is classified as unsafe during gestation due to endocrine axis disruption potential.
Fetal toxicity and teratogenic considerations
Interference with fetal neuro-endocrine development is plausible, and teratogenic influence cannot be ruled out.
Contraindication during breastfeeding and milk suppression concerns
The medicine is contraindicated during lactation. Hormonal modulation may suppress lactogenesis and may transfer into milk.
Administration to Children and Adolescents
Lack of established safety data in pediatric populations
Research remains insufficient to confirm consistent safety in younger cohorts.
Limited clinical justification except in rare oncology-related cases
Pediatric use is typically confined to oncology-specialist protocols.
Monitoring parameters for growth and endocrine imbalance
Growth trajectory, pubertal progression, and metabolic panels should be periodically evaluated if therapy is employed.
Overdosage and Toxicity Management
Expected overdose manifestations (electrolyte imbalance, adrenal crisis, severe hyperglycemia)
Overdose may lead to extreme glucocorticoid-like physiology. • Electrolyte derangements • Adrenal collapse • Potentially fatal hyperglycemia
Emergency stabilization and supportive management
First-line intervention involves cardiorespiratory stabilization, glucose correction, and supportive fluids.
Activated charcoal and elimination strategies
Activated charcoal may be considered acutely if ingestion is recent. Hormonal clearance is largely hepatic and supportive in nature.
Handling and Storage Precautions
Recommended temperature range and stability conditions
Storage should follow standard room temperature stability zones unless otherwise manufacturer-specified.
Packaging integrity and moisture protection
Intact blister packs or sealed containers should be maintained to avoid humidity-related degradation.
Safe handling measures in clinical settings for hormonal agents
Hormonal products warrant mindful handling. Protective gloves may be used during bulk dispensing and inventory preparation. ```