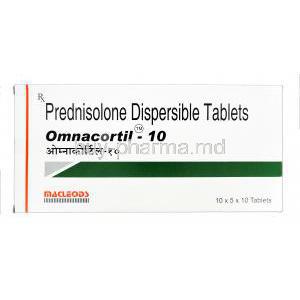
Introduction to Omnacortil
Omnacortil is a widely prescribed corticosteroid containing Prednisolone as its active pharmaceutical ingredient. It is a synthetic glucocorticoid designed to replicate the actions of natural cortisol, a hormone essential for regulating inflammation, metabolism, and immune response.
As a member of the systemic corticosteroid class, Omnacortil plays a pivotal role in managing a wide spectrum of inflammatory, allergic, and autoimmune disorders. Its potent anti-inflammatory and immunosuppressive properties make it indispensable in modern clinical practice.
Historically, Prednisolone emerged in the mid-20th century as a refined derivative of cortisone, offering improved efficacy and fewer mineralocorticoid effects. Over time, it has become a cornerstone therapy in both acute and chronic medical conditions. Pharmacologically, it is classified among intermediate-acting glucocorticoids, balancing strong anti-inflammatory potency with moderate duration of action.
Composition and Formulation
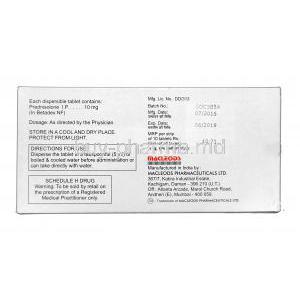
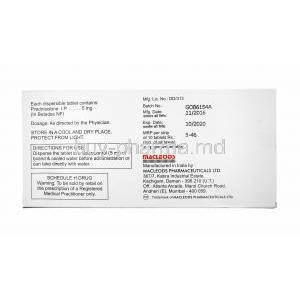
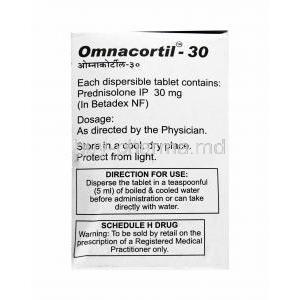
The primary component of Omnacortil is Prednisolone, a corticosteroid with glucocorticoid activity. It is formulated for systemic absorption and optimal therapeutic action.
- Active ingredient: Prednisolone, a synthetic glucocorticoid with potent anti-inflammatory and immunosuppressive activity.
- Available dosage forms: Tablets (5 mg, 10 mg, 20 mg, 40 mg), oral syrup, and injectable formulations.
- Excipients: May include lactose monohydrate, microcrystalline cellulose, maize starch, and magnesium stearate.
- Equivalent brands: Prednisone (prodrug), Deltacortril, and other prednisolone-based corticosteroids in global markets.
Mechanism of Action
Prednisolone exerts its effects through complex genomic and non-genomic pathways. It binds to cytoplasmic glucocorticoid receptors, forming a receptor-ligand complex that translocates into the cell nucleus. There, it modulates gene transcription to suppress pro-inflammatory cytokines such as interleukin-1, interleukin-6, and TNF-α.
- Inhibits phospholipase A2 and cyclooxygenase-2 (COX-2) activity, reducing prostaglandin and leukotriene synthesis.
- Stabilizes lysosomal membranes and reduces capillary permeability, minimizing tissue inflammation.
- Suppresses immune cell migration and activation, preventing excessive immune response.
This multifaceted mechanism underpins its therapeutic use across respiratory, dermatologic, hematologic, and neurological systems.
Therapeutic Uses
4.1 Primary Indications
Omnacortil is utilized in a diverse array of medical conditions, including:
- Allergic disorders: Asthma, dermatitis, rhinitis, and urticaria.
- Autoimmune diseases: Systemic lupus erythematosus, rheumatoid arthritis.
- Endocrine disorders: Adrenal insufficiency, congenital adrenal hyperplasia.
- Hematologic diseases: Autoimmune hemolytic anemia, idiopathic thrombocytopenia.
- Pulmonary disorders: Chronic obstructive pulmonary disease (COPD), sarcoidosis.
- Gastrointestinal inflammation: Ulcerative colitis, Crohn’s disease.
- Neurological conditions: Multiple sclerosis relapse, Bell’s palsy.
- Dermatologic therapy: Psoriasis, eczema, and other severe inflammatory rashes.
4.2 Off-label and Adjunctive Uses
- Nephrotic syndrome: Controls proteinuria and inflammation in renal conditions.
- Transplant medicine: Prevents graft rejection by immunosuppression.
- Oncology: Supportive therapy in leukemia, lymphoma, and multiple myeloma.
- Emergency care: Adjunct in acute allergic reactions and anaphylaxis.
- COVID-19 management: Reduces cytokine storm-related inflammation (off-label).
- Ophthalmology: Used in uveitis, optic neuritis, and ocular inflammatory states.
Dosage and Administration
Dosage of Omnacortil is individualized based on clinical condition and therapeutic response. It should be administered under medical supervision with periodic reassessment.
- Typical adult dose: 5–60 mg per day, divided or single morning dose.
- Children: Dose based on body weight and disease severity.
- Route of administration: Oral tablets, syrup, or parenteral injection.
- Morning administration: Recommended to align with the body’s circadian cortisol rhythm.
- Tapering: Gradual reduction required to avoid adrenal insufficiency.
- Missed dose: Take as soon as remembered unless close to next scheduled dose.
Side Effects
6.1 Common Side Effects
- Increased appetite leading to weight gain.
- Insomnia, mood fluctuations, or mild irritability.
- Stomach upset, nausea, or dyspepsia.
- Water retention causing facial puffiness.
6.2 Serious Adverse Reactions
- Adrenal suppression and Cushingoid features.
- Musculoskeletal complications such as osteoporosis and muscle atrophy.
- Metabolic disturbances including hyperglycemia and hypertension.
- Peptic ulcers and gastrointestinal bleeding.
- Impaired immune defense, predisposing to infections.
- Ophthalmic issues like glaucoma and cataract formation.
- Psychiatric manifestations: depression, mania, or psychosis.
Drug Interactions
- NSAIDs and anticoagulants: Heightened risk of gastric bleeding.
- CYP3A4 inhibitors: (e.g., ketoconazole, erythromycin) increase Prednisolone concentration.
- Vaccines: Live vaccines contraindicated during therapy.
- Diuretics and hypoglycemics: Possible interference with electrolyte and glucose control.
- Anticonvulsants and oral contraceptives: May alter prednisolone metabolism or potency.
Warnings and Important Precautions
- Avoid abrupt cessation after prolonged use to prevent adrenal crisis.
- Minimize exposure to contagious diseases such as chickenpox and measles.
- Monitor vital parameters: blood pressure, blood sugar, and bone mineral density.
- Patients with latent infections (e.g., tuberculosis) require prophylactic management.
- Periodic eye check-ups recommended for long-term users.
- Psychological assessment for mood or behavioral alterations during therapy.
Contraindications
- Known hypersensitivity to Prednisolone or any component of Omnacortil.
- Presence of systemic fungal infections.
- Severe or uncontrolled hypertension and diabetes mellitus.
- Active peptic ulcer disease or gastrointestinal perforation.
- Concurrent administration of live or attenuated vaccines.
- Use with caution in tuberculosis or systemic infections without antimicrobial cover.
Omnacortil remains a cornerstone in corticosteroid therapy, providing rapid symptom control and clinical improvement when administered responsibly under medical guidance.
Careful Administration and Monitoring
The administration of Omnacortil (Prednisolone) requires meticulous medical supervision, especially in prolonged therapy. Periodic assessments ensure optimal therapeutic response while minimizing systemic complications. Monitoring should be customized based on patient health status, dosage, and duration of treatment.
- Adrenal function and electrolyte balance: Long-term corticosteroid therapy can suppress the hypothalamic-pituitary-adrenal (HPA) axis. Regular evaluation of cortisol levels and serum electrolytes such as sodium and potassium is crucial to prevent adrenal insufficiency and electrolyte imbalance.
- Bone density and growth monitoring: Prolonged corticosteroid exposure can cause osteopenia or osteoporosis. Bone mineral density scans and growth tracking (especially in children) are recommended for early detection of skeletal effects.
- Hepatic and renal adjustment: Dose modification may be necessary in patients with hepatic or renal dysfunction to prevent excessive systemic accumulation of Prednisolone.
- Ophthalmologic assessment: Long-term users should undergo periodic eye examinations to detect glaucoma, cataracts, or optic nerve damage early.
- Infection surveillance: Corticosteroids increase susceptibility to bacterial, viral, and fungal infections. Prophylactic measures and vaccination planning are essential to mitigate infection risk.
Administration in Special Populations
11.1 Elderly Patients
Elderly individuals exhibit physiological changes that heighten the sensitivity to corticosteroids. Reduced hepatic metabolism and renal clearance necessitate cautious dosing and vigilant monitoring.
- Clearance considerations: Diminished organ function can prolong drug half-life, increasing the risk of adverse events.
- Enhanced vulnerability: Older adults face a greater risk of osteoporosis, hypertension, glucose intolerance, and muscle weakness during prolonged corticosteroid use.
- Therapeutic approach: Employ the minimal effective dose, taper gradually, and ensure concurrent calcium and vitamin D supplementation to preserve bone health.
11.2 Pregnant and Nursing Women
Prednisolone should be prescribed during pregnancy only when the potential benefit outweighs possible fetal risks. Although it crosses the placental barrier, its teratogenic potential is dose-dependent and generally low when used short term.
- Fetal considerations: Chronic maternal exposure may impair fetal growth or cause adrenal suppression in the neonate.
- Lactation: Small quantities of Prednisolone are excreted in breast milk, which may lead to mild adrenal suppression in the infant. Short-term or low-dose therapy is generally compatible with breastfeeding.
- Clinical guidance: Monitor both mother and infant for growth abnormalities, adrenal suppression, and developmental milestones during and after treatment.
11.3 Pediatric Administration
Children are particularly sensitive to the systemic effects of corticosteroids. Prolonged use demands rigorous oversight to prevent growth inhibition and hormonal imbalances.
- Growth suppression: Chronic therapy may reduce growth velocity and impair skeletal development; hence, the lowest effective dose for the shortest possible duration should be maintained.
- Dosage considerations: Pediatric dosing should be strictly weight-based and re-evaluated regularly as the child grows.
- Infection and immunization: Live vaccines should be avoided during treatment. Preventive hygiene and timely management of infections are essential.
Overdosage
Accidental or intentional overdose of Prednisolone can lead to acute or chronic systemic toxicity. The clinical presentation varies with dosage and duration.
- Symptoms: Edema due to fluid retention, hypertension, electrolyte disturbances (hypokalemia, hypernatremia), and hyperglycemia are common manifestations. Severe cases may show adrenal crisis upon abrupt withdrawal.
- Management: There is no specific antidote. Treatment includes gradual dose reduction, supportive care, correction of electrolyte imbalances, and close hemodynamic monitoring.
- Prevention: Educate patients on the importance of prescribed dosage adherence and never self-adjusting corticosteroid intake.
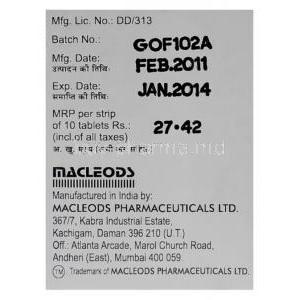
Handling and Storage
Proper handling and storage preserve the potency and safety of Omnacortil formulations. Exposure to adverse environmental conditions can degrade the medication and compromise efficacy.
- Temperature control: Store at 15°C–30°C (59°F–86°F) in a cool, dry place.
- Protection from elements: Keep away from direct sunlight, heat, and moisture to prevent decomposition.
- Shelf life: Observe expiry dates on packaging and discard unused medication after expiration.
- Safe handling: Avoid contamination by using clean, dry hands or utensils, especially with oral syrups or suspensions.
- Disposal: Dispose of expired or unused medication through approved pharmaceutical waste systems to protect the environment.
Handling Precautions and Patient Counseling
Comprehensive patient education enhances safety and therapeutic compliance during Omnacortil therapy. Continuous communication between patient and healthcare provider is essential for optimal outcomes.
- Medication tapering: Abrupt discontinuation after long-term use may precipitate adrenal crisis. Gradual tapering under medical guidance is mandatory.
- Follow-up and monitoring: Regular clinical evaluations, blood tests, and blood pressure monitoring help detect emerging side effects early.
- Vaccination and infection caution: Avoid live vaccines during therapy and maintain infection control precautions in daily life.
- Adherence: Patients should take medication precisely as prescribed to maintain stable blood levels and therapeutic effect.
- Reporting adverse effects: Promptly report signs of infection, visual disturbances, severe mood changes, or gastrointestinal pain.
Responsible use of Omnacortil ensures maximum therapeutic benefit with minimal systemic risk. Through diligent monitoring, individualized dosing, and patient education, corticosteroid therapy remains an essential yet safely manageable treatment option.