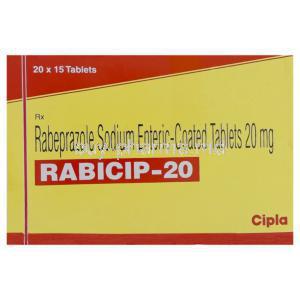
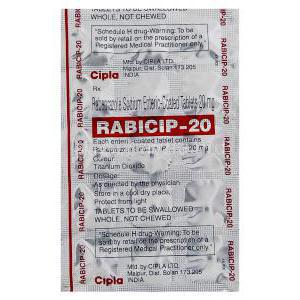
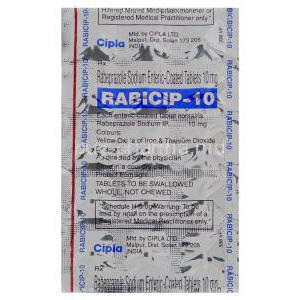
Rabeprazole
Uses
Rabicip, Rabeprazole Sodium is used in the treatment of acidity,intestinal ulcers, heartburn and stomach ulcers.
How it Works
Rabicip, Rabeprazole Sodium works by stopping the cells in the lining of the stomach from producing too much acid, and this helps to prevent ulcers from forming, or assists the healing process where damage has already occurred. Rabicip, Rabeprazole Sodium works by decreasing the amount of acid, and this can also help to reduce the symptoms of acid reflux disease, such as acidity, heartburn, intestinal ulcers and stomach ulcers.
Common Side effects
Patients who take Rabicip, Rabeprazole Sodium may suffer from such side effects;
Nausea,
Abdominal pain,
Vomiting,
Constipation,
Diarrhoea,
Flatulence