Introduction to Sazo DR (Sulfasalazine)
Overview of Sazo DR as a Disease-Modifying Antirheumatic Drug (DMARD)
Sazo DR, containing sulfasalazine, is categorized as a disease-modifying antirheumatic drug (DMARD). Unlike symptomatic treatments, DMARDs aim to alter the underlying disease process, reducing inflammation and preventing long-term joint damage. This medication has been a cornerstone in the management of chronic autoimmune conditions where conventional painkillers fall short.
History and Clinical Development of Sulfasalazine
Sulfasalazine was originally developed in the 1940s as a hybrid compound that combined antibacterial and anti-inflammatory components. It has since been rigorously studied and repurposed to treat conditions such as rheumatoid arthritis and inflammatory bowel disease, demonstrating its enduring therapeutic relevance across decades.
Therapeutic Importance in Autoimmune and Inflammatory Disorders
Autoimmune and chronic inflammatory diseases often lead to progressive tissue destruction. Sulfasalazine’s ability to regulate immune responses has made it indispensable in conditions like rheumatoid arthritis and ulcerative colitis. Its use has helped patients avoid disability, improve quality of life, and maintain long-term remission.
Composition and Formulation
Active Ingredient: Sulfasalazine
The principal compound is sulfasalazine, a conjugate of sulfapyridine and 5-aminosalicylic acid. This unique structure allows dual activity once metabolized in the body.
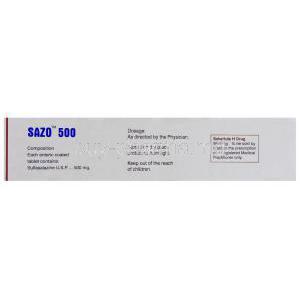
Available Dosage Strengths and Delayed-Release (DR) Formulation
Sazo DR is typically available in 500 mg delayed-release tablets, engineered to withstand gastric acidity and release the drug in the intestine for maximum effect.
Inactive Ingredients and Excipients
The formulation contains inert components such as cellulose derivatives, starch, and binding agents that ensure tablet stability and controlled release.
Pharmaceutical Class and Mechanism Classification
Sulfasalazine belongs to the class of aminosalicylates with immunomodulatory properties. It is both anti-inflammatory and antimicrobial in action, setting it apart from conventional NSAIDs.
Mechanism of Action: How Sulfasalazine Works
Breakdown into Sulfapyridine and 5-Aminosalicylic Acid (5-ASA)
In the colon, sulfasalazine is cleaved by bacterial enzymes into sulfapyridine and 5-ASA. Each metabolite exerts distinct therapeutic effects: sulfapyridine contributes to systemic immunomodulation, while 5-ASA reduces local intestinal inflammation.
Anti-Inflammatory and Immunomodulatory Effects
The drug suppresses pro-inflammatory mediators while modulating immune cell activity. This dual action allows it to control systemic as well as localized inflammation.
Impact on Prostaglandin and Cytokine Pathways
Sulfasalazine inhibits cyclooxygenase activity and reduces prostaglandin synthesis. It also downregulates cytokines such as TNF-alpha and interleukin-1, pivotal drivers of chronic inflammation.
Role in Modulating Gut Microbiota and Immune Response
Evidence suggests sulfasalazine alters intestinal microbiota composition, which may indirectly reduce immune hyperreactivity. This connection between gut health and systemic inflammation adds another layer of therapeutic benefit.
Medical Uses of Sazo DR
FDA-Approved Indications
- Rheumatoid Arthritis (RA): Slows disease progression, reduces joint swelling, and prevents erosive damage.
- Juvenile Idiopathic Arthritis (JIA): Effective in children with persistent arthritis unresponsive to NSAIDs.
- Ulcerative Colitis (UC): Induces remission and maintains long-term symptom control.
- Ankylosing Spondylitis: Provides relief from spinal inflammation and stiffness.
Off-Label Uses
- Crohn’s Disease: Used in mild to moderate forms of inflammatory bowel disease.
- Psoriatic Arthritis: Helps alleviate joint and skin-related manifestations.
- Reactive Arthritis: Reduces joint inflammation following infections.
- Chronic Inflammatory Bowel Diseases: Utilized in specific cases where conventional therapy is insufficient.
- Other Autoimmune Conditions: Occasionally prescribed for off-label management of systemic inflammatory disorders.
Dosage and Administration
Standard Adult Dosing for RA, UC, and Ankylosing Spondylitis
Typical adult doses begin at 500 mg once or twice daily, with gradual escalation up to 2–3 g per day depending on tolerance and therapeutic response.
Pediatric Dosage Guidelines
For juvenile arthritis, dosing is weight-based, often ranging from 30 to 50 mg/kg/day divided into multiple doses.
Gradual Dose Escalation to Minimize Intolerance
Dosing begins low and increases slowly to minimize nausea and gastrointestinal discomfort. This titration method improves patient adherence.
Administration with Food or Water
Tablets should be taken with meals or a full glass of water to reduce stomach irritation and enhance absorption.
Duration of Therapy and Monitoring Requirements
Long-term use is common, often extending for years. Regular laboratory monitoring of blood counts, liver function, and renal function is recommended throughout treatment.
Side Effects of Sulfasalazine
Common Side Effects
- Nausea, vomiting, and gastrointestinal upset
- Headache and dizziness
- Loss of appetite
- Skin rash and itching
Less Common but Significant Side Effects
- Photosensitivity reactions leading to exaggerated sunburn
- Orange discoloration of urine, sweat, and skin
- Reversible reduction in sperm count in men
Serious Adverse Reactions
- Bone marrow suppression, manifesting as anemia or leukopenia
- Liver toxicity including hepatitis
- Severe hypersensitivity reactions such as Stevens-Johnson syndrome
- Pulmonary toxicity with cough or breathlessness
Drug Interactions
Interactions with Methotrexate and Other DMARDs
Co-administration with methotrexate may enhance therapeutic benefit but requires monitoring due to potential additive toxicity.
Effect on Digoxin Absorption
Sulfasalazine can decrease digoxin absorption, potentially reducing its efficacy in heart failure or arrhythmia patients.
Warfarin and Anticoagulant Interaction Risks
It may potentiate the effects of anticoagulants, increasing the risk of bleeding. Frequent INR monitoring is essential.
Antibiotics Reducing Efficacy
Broad-spectrum antibiotics can disrupt gut bacteria responsible for sulfasalazine metabolism, lowering drug activity.
Alcohol Interaction
Concurrent alcohol intake increases the risk of hepatotoxicity and gastrointestinal irritation. Patients are advised to limit or avoid alcohol consumption during therapy.
Warnings and Important Precautions
Need for Regular Blood Tests
Patients on sulfasalazine require frequent laboratory monitoring. Complete blood counts (CBC), liver function panels, and renal profiles must be performed at baseline and at regular intervals. This ensures early detection of hematologic abnormalities, hepatic dysfunction, or renal impairment.
Risk of Stevens-Johnson Syndrome (SJS) and Severe Skin Reactions
Rare but life-threatening dermatological reactions can occur. Stevens-Johnson Syndrome and toxic epidermal necrolysis may manifest with fever, mucosal lesions, and widespread blistering. Immediate discontinuation is mandatory if skin reactions progress beyond mild rash.
Allergic Reactions in Sulfa-Sensitive Patients
Individuals with a history of hypersensitivity to sulfonamides are at heightened risk of allergic manifestations. Reactions may include:
- Urticaria and pruritus
- Respiratory distress
- Anaphylaxis in rare cases
Risk of Infertility (Male Reversible)
Men may experience reversible oligospermia during treatment. Fertility typically returns within months after discontinuation, but counseling should be provided for those planning families.
Caution in G6PD Deficiency
Patients with glucose-6-phosphate dehydrogenase deficiency are predisposed to hemolytic anemia. Use with caution, accompanied by vigilant monitoring of hemoglobin levels.
Contraindications
- Known Hypersensitivity: Contraindicated in patients allergic to sulfasalazine, sulfonamides, or salicylates.
- Severe Liver or Renal Impairment: Risk of accumulation and toxicity makes administration unsafe.
- Porphyria: May trigger acute porphyric attacks due to enzyme inhibition.
- Intestinal or Urinary Obstruction: Blockages can impede drug passage and elevate adverse outcomes.
Careful Administration Guidelines
Titration Strategies to Reduce Gastrointestinal Intolerance
Initiating treatment at low doses and gradually escalating reduces nausea and abdominal discomfort. This phased approach enhances adherence.
Adequate Hydration to Prevent Crystalluria
Patients should maintain sufficient fluid intake to avoid urinary crystallization and related complications such as kidney stones.
Use of Folic Acid Supplementation
Sulfasalazine interferes with folate absorption. Supplementation is recommended to prevent megaloblastic anemia and maintain healthy cell division.
Baseline and Periodic Lab Monitoring
Laboratory testing should be conducted at therapy initiation, followed by intervals of every 2–4 weeks initially, then extended as clinically appropriate. Monitoring includes CBC, hepatic enzymes, and renal markers.
Use in Special Populations
Administration to Elderly
Elderly patients often present with multiple comorbidities and polypharmacy. Close surveillance for hepatotoxicity and bone marrow suppression is crucial. Dose adjustments may be required.
Administration to Pregnant Women
Sulfasalazine is classified as Category B. While not linked to teratogenicity, it reduces folate levels, necessitating supplementation. Caution is advised in late pregnancy due to risk of neonatal jaundice.
Administration to Nursing Mothers
The drug and its metabolites are excreted in breast milk. Potential risks include:
- Diarrhea in the infant
- Jaundice in neonates, particularly those with G6PD deficiency
Breastfeeding should be carefully evaluated against maternal benefit.
Administration to Children
Indicated for juvenile idiopathic arthritis and inflammatory bowel disease. Pediatric dosing is weight-based and requires meticulous adjustment. Children should be monitored for growth parameters, tolerance, and laboratory changes.
Overdosage
Signs and Symptoms
Excessive intake may lead to gastrointestinal distress (nausea, vomiting, abdominal pain), central nervous system effects (drowsiness, seizures), and hematologic abnormalities (methemoglobinemia, anemia).
Immediate Supportive Management
Supportive care is essential. Key interventions include fluid resuscitation, electrolyte correction, and vital sign stabilization.
Gastric Lavage and Activated Charcoal
In acute ingestion, gastric lavage and administration of activated charcoal may reduce absorption. Timing of intervention is critical.
Hemodialysis Considerations
Hemodialysis may aid in eliminating metabolites, though its efficacy is variable. It remains an option in severe toxicity cases.
Storage and Handling Precautions
Recommended Storage Conditions
Tablets should be stored at controlled room temperature, shielded from moisture, direct light, and excessive heat. Proper storage preserves stability and potency.
Safe Handling to Avoid Contamination
Tablets should be kept in original packaging until use. Care should be taken to prevent accidental contact with broken or crushed tablets, especially by caregivers.
Expiry and Proper Disposal
Expired medications lose efficacy and may cause harm. Disposal should follow local pharmaceutical waste guidelines to prevent environmental contamination.
Patient Counseling
Patients should be counseled to:
- Adhere strictly to prescribed schedules
- Report any unusual symptoms immediately
- Store the medication away from children and pets