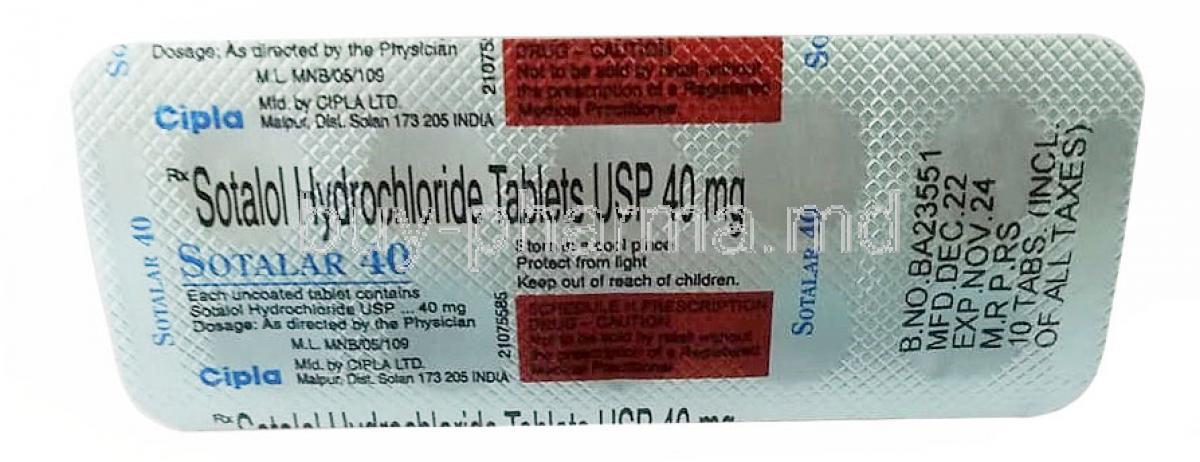
Introduction to Sotalar (Sotalol)
Overview of Sotalar as an Antiarrhythmic and Beta-Blocker
Sotalar, known generically as sotalol, is a medication with a distinctive dual pharmacological profile. It functions both as a non-selective beta-adrenergic blocker and as a Class III antiarrhythmic agent. This unique combination enables it to slow down abnormal cardiac rhythms while simultaneously reducing the workload on the heart.
- Stabilizes erratic electrical impulses in the myocardium
- Reduces the frequency of irregular or rapid heartbeats
- Improves cardiac efficiency by lowering oxygen demand
Brief History and Clinical Significance in Cardiology
Since its introduction in the late 20th century, sotalol has held a prominent place in cardiology. It was one of the first medications to demonstrate effectiveness in both atrial and ventricular arrhythmias, significantly lowering the risk of sudden cardiac death in high-risk patients. Its clinical importance stems from decades of usage in hospitals worldwide.
Differences Between Brand Sotalar and Generic Sotalol
The branded formulation, Sotalar, provides the same therapeutic efficacy as its generic counterpart, sotalol hydrochloride. The primary differences lie in manufacturing processes, inactive components, and branding. Both options, however, must meet strict regulatory standards ensuring comparable safety and effectiveness.
Composition and Formulation
Active Ingredient: Sotalol Hydrochloride
The active pharmaceutical ingredient is sotalol hydrochloride, a crystalline compound that exerts potent effects on the electrical conduction system of the heart.
Available Strengths and Dosage Forms
Sotalar is commercially available in various oral strengths, typically 80 mg, 120 mg, and 160 mg tablets. In specialized hospital environments, intravenous formulations are used to manage acute arrhythmic episodes.
Inactive Ingredients and Excipients
Each tablet also contains pharmacologically inactive compounds such as microcrystalline cellulose, magnesium stearate, and lactose monohydrate. These excipients ensure tablet stability, absorption, and patient tolerability.
Mechanism of Action: How Sotalol Works
Dual Action: Class II Beta-Blocker and Class III Antiarrhythmic
Sotalol exhibits a rare duality. As a Class II beta-blocker, it inhibits adrenergic stimulation, lowering heart rate and contractility. As a Class III antiarrhythmic, it prolongs the repolarization phase by blocking potassium channels, stabilizing cardiac rhythm.
Effects on Heart Rhythm and Electrical Activity
The drug lengthens the refractory period of cardiac tissue, suppressing abnormal re-entrant circuits that trigger arrhythmias. This makes it especially valuable in controlling both atrial fibrillation and ventricular tachycardia.
Role in Controlling Heart Rate and Preventing Arrhythmias
By slowing atrioventricular conduction and reducing excitability, sotalol maintains sinus rhythm in patients prone to relapse. It minimizes the likelihood of arrhythmic recurrences that can compromise cardiac output and quality of life.
Approved Medical Uses of Sotalar
Treatment of Life-Threatening Ventricular Arrhythmias
Sotalar is indicated for the suppression of sustained ventricular tachycardia, a condition that can progress to ventricular fibrillation and sudden cardiac arrest if untreated.
Maintenance of Normal Sinus Rhythm in Atrial Fibrillation or Atrial Flutter
Patients with recurrent atrial fibrillation or flutter benefit from sotalol’s rhythm-stabilizing capacity. It reduces hospitalizations and improves long-term outcomes by decreasing relapse frequency.
Prevention of Recurrent Ventricular Tachycardia
In individuals with structural heart disease, sotalol prevents recurrent ventricular tachycardia, offering protection from hemodynamic instability and fatal arrhythmias.
Use in Patients with Symptomatic Arrhythmias
Sotalol is often prescribed for patients who experience palpitations, dizziness, or syncope related to irregular cardiac rhythms. Its use restores rhythm control and reduces debilitating symptoms.
Off-Label Uses of Sotalol
Management of Supraventricular Tachycardia (SVT)
Sotalol has demonstrated efficacy in the management of SVT, where rapid atrial impulses overwhelm normal conduction pathways.
Pediatric Use in Congenital Arrhythmias
Though not formally approved, sotalol is sometimes used under specialist supervision to treat congenital arrhythmic disorders in children.
Adjunct Therapy in Long QT Syndrome Management
Sotalol may be used as part of a therapeutic strategy in long QT syndrome, reducing susceptibility to dangerous ventricular arrhythmias.
Potential Role in Other Rhythm Disturbances
Research continues to explore sotalol’s benefits in less common arrhythmic disorders, broadening its therapeutic potential beyond official approvals.
Dosage and Administration Guidelines
Standard Adult Dosing Schedules
Initial therapy generally begins at 80 mg twice daily, with gradual titration based on patient response and tolerance. Some cases may require 160–320 mg per day.
Dose Titration and Monitoring Requirements
Careful titration is mandatory due to the risk of proarrhythmia. Patients typically require electrocardiographic monitoring during dose adjustments to detect QT interval prolongation.
Adjustments in Renal Impairment
Because sotalol is primarily excreted renally, dose reductions are necessary in patients with impaired kidney function. Creatinine clearance levels guide precise dosing.
Intravenous Administration in Hospital Settings
In emergency or acute arrhythmic crises, intravenous sotalol is administered under continuous monitoring to rapidly stabilize cardiac rhythm.
Missed Dose Instructions and Patient Guidance
If a dose is missed, patients are advised to take it as soon as remembered unless it is close to the time of the next dose. Doubling doses to compensate is contraindicated due to heightened arrhythmic risk.
Side Effects of Sotalol
Overview of Safety Profile
Sotalol is widely prescribed for arrhythmia control, but like all potent cardiac medications, it carries a significant safety profile. Its dual role as a beta-blocker and antiarrhythmic increases its therapeutic value, yet this same profile predisposes patients to both predictable and unpredictable side effects. Understanding these outcomes helps clinicians and patients balance efficacy with tolerability.
Distinction Between Common and Serious Side Effects
Adverse effects of sotalol can be divided into common, generally manageable symptoms and rare but potentially life-threatening complications. Common effects often improve with continued use or dosage adjustment, while serious reactions necessitate urgent medical care and, at times, discontinuation of therapy.
Common Side Effects
Fatigue, Dizziness, and Headache
These neurological complaints are among the most frequently reported. Patients may describe difficulty concentrating, mild disorientation, or tension-type headaches. Such symptoms usually resolve as the body adapts to therapy but may persist in sensitive individuals.
Nausea, Vomiting, and Gastrointestinal Upset
Sotalol can disturb gastrointestinal function, leading to nausea, occasional vomiting, and abdominal discomfort. Small, frequent meals and adequate hydration often alleviate these symptoms.
Cold Extremities and Mild Bradycardia
Reduced peripheral circulation may result in sensations of cold hands and feet. Mild slowing of the heart rate, known as bradycardia, is a direct pharmacological effect but becomes concerning only when severe or symptomatic.
Serious and Rare Adverse Reactions
Risk of Torsades de Pointes and Other Proarrhythmias
Prolongation of the QT interval is a well-documented effect of sotalol. This can precipitate torsades de pointes, a potentially lethal arrhythmia requiring immediate intervention. Continuous monitoring during initiation is recommended.
Severe Bradycardia or Heart Block
In susceptible patients, sotalol may suppress cardiac conduction excessively, leading to profound bradycardia or atrioventricular block. These conditions demand urgent medical management, often involving drug discontinuation or pacemaker support.
Hypotension and Syncope
Marked drops in blood pressure can cause dizziness, fainting, or collapse. Such episodes increase the risk of injury and may signal the need for dose reduction.
Worsening Heart Failure
Although sometimes used in patients with cardiac dysfunction, sotalol can exacerbate pre-existing heart failure by reducing contractility. Monitoring fluid balance, weight, and cardiac output is critical during therapy.
Drug Interactions with Sotalol
Interactions with Other Antiarrhythmic Drugs
Concurrent use with Class Ia or Class III antiarrhythmics significantly raises the risk of QT prolongation and dangerous arrhythmias. Such combinations are typically avoided.
Effects of Concomitant Beta-Blocker Use
Administering sotalol alongside other beta-blockers enhances bradycardic and hypotensive effects, potentially leading to cardiovascular collapse.
Risk with QT-Prolonging Medications
Antidepressants, antipsychotics, and certain antibiotics that prolong the QT interval should be used with extreme caution in patients taking sotalol.
Food and Alcohol Interactions
Alcohol intensifies dizziness and fainting, while abrupt dietary changes in electrolyte balance may alter sotalol’s arrhythmic risk profile. Patients are advised to maintain consistent dietary habits.
Warnings and Important Precautions
Black Box Warning Regarding Proarrhythmia
Sotalol carries a boxed warning for its potential to induce proarrhythmia, underscoring the necessity of inpatient monitoring during therapy initiation.
Need for Hospitalization During Initiation and Dose Adjustment
Patients starting sotalol require electrocardiographic monitoring for at least three days to ensure QT stability and prevent life-threatening arrhythmias.
Risks in Patients with Structural Heart Disease
Structural abnormalities increase susceptibility to conduction disturbances. Physicians must weigh the risks carefully before prescribing sotalol in these populations.
Monitoring of Electrolyte Balance
Serum potassium and magnesium must be maintained within normal limits. Imbalances dramatically increase the probability of torsades de pointes.
Contraindications of Sotalol
Known Hypersensitivity to Sotalol Hydrochloride
Patients with documented allergic reactions to sotalol or its excipients should not receive this medication.
Baseline QT Prolongation
Individuals with a pre-existing prolonged QT interval face elevated risks of ventricular arrhythmias and should avoid sotalol therapy.
Severe Renal Impairment Without Monitoring
Since sotalol is eliminated renally, impaired kidney function without proper dose adjustment poses severe toxicity risks.
Asthma or Severe Chronic Obstructive Pulmonary Disease
Non-selective beta-blockade can trigger bronchospasm, rendering sotalol contraindicated in such patients.
Uncontrolled Heart Failure
Sotalol should not be initiated in decompensated or unstable heart failure due to the danger of further cardiac suppression.
Careful Administration Considerations
Gradual Withdrawal to Avoid Rebound Effects
Sudden discontinuation can provoke rebound tachycardia, hypertension, or arrhythmias. Tapering is essential.
Caution in Diabetic Patients
Sotalol may mask hypoglycemic symptoms such as tachycardia and tremors, complicating diabetes management.
Considerations in Patients with Thyroid Disease
Hyperthyroidism may be concealed by sotalol, delaying diagnosis and treatment. Careful endocrine assessment is warranted.
Polypharmacy Risks in Elderly Patients
Elderly individuals often use multiple medications, raising the risk of adverse drug interactions and necessitating vigilant supervision.
Administration in Special Populations
Use in Elderly Patients
Older adults demonstrate heightened sensitivity to bradycardia and hypotension. Lower starting doses and closer surveillance are typically required.
Use in Pregnant Women and Nursing Mothers
While sotalol may be considered during pregnancy for life-threatening arrhythmias, it crosses the placenta and carries potential risks to the fetus. It is also excreted in breast milk, where it may affect neonatal cardiac and metabolic function. Clinical judgment should guide therapy in these scenarios.
Use in Children and Adolescents
Pediatric data is limited, but sotalol has been employed under strict specialist supervision for congenital arrhythmias. Dosing must be carefully tailored to body weight and age.
Overdosage and Emergency Management
Symptoms of Sotalol Overdose
Overdose can manifest as profound bradycardia, severe hypotension, prolonged QT intervals, and malignant arrhythmias.
Immediate Medical Interventions and Treatment Protocols
Initial steps include discontinuation, gastric decontamination, and supportive care. Atropine, isoproterenol, and temporary pacing may be necessary.
Role of Hemodialysis in Severe Overdose
Because sotalol is renally excreted, hemodialysis can effectively reduce plasma concentrations during toxic overdoses.
Storage and Handling Precautions
Recommended Storage Conditions
Sotalol should be stored at controlled room temperature, away from excess humidity and light exposure, to preserve its stability.
Safe Handling and Disposal of Unused Medication
Unused tablets should be disposed of responsibly, following pharmaceutical waste protocols. Accidental ingestion poses severe health risks.
Special Instructions for Hospital Pharmacies and IV Formulations
Intravenous sotalol requires careful preparation in sterile environments. Hospital pharmacies must implement precise handling guidelines to prevent dosing errors.