Introduction to Sotalol
Sotalol is a distinctive medication that belongs to the class of non-selective beta-blockers while also exhibiting Class III antiarrhythmic properties. This rare dual mechanism makes it invaluable in managing complex rhythm disturbances. Unlike many conventional agents, Sotalol exerts a profound influence on both adrenergic activity and cardiac electrical stability.
The drug was developed in the latter half of the 20th century and gradually gained worldwide approval for clinical use, particularly in the treatment of severe arrhythmias. Over time, it has become an essential part of the cardiologist’s arsenal, especially for patients at high risk of sudden cardiac events.
Its therapeutic importance lies in its ability to suppress abnormal heart rhythms, maintain sinus rhythm, and reduce the recurrence of potentially life-threatening arrhythmias. By addressing both rate and rhythm, Sotalol provides an advanced solution where other agents may fail.
Composition and Formulations
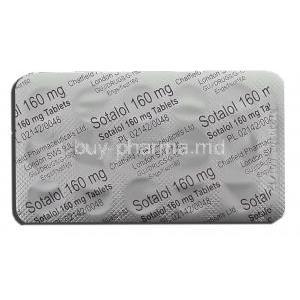
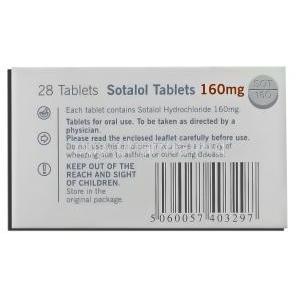
The active ingredient is Sotalol hydrochloride, a crystalline compound with potent antiarrhythmic activity. It is formulated in various strengths to suit individualized therapy.
- Oral tablets: Commonly available in strengths such as 40 mg, 80 mg, and 160 mg.
- Intravenous (IV) formulations: Used in acute hospital settings for rapid stabilization.
- Global availability: Sold under multiple brand names alongside generic versions, ensuring accessibility worldwide.
How Sotalol Works (Mechanism of Action)
Sotalol exerts a unique dual mechanism:
- Beta-adrenergic blocking activity (Class II effect): By blocking beta receptors, it decreases heart rate, lowers myocardial oxygen demand, and reduces excitability.
- Potassium channel blockade (Class III effect): Sotalol prolongs the action potential duration and refractoriness, which stabilizes electrical conduction and prevents arrhythmias.
Through these combined effects, the drug is capable of both slowing the heart rate and reducing the likelihood of abnormal electrical re-entry circuits, resulting in rhythm stabilization.
Approved Medical Uses of Sotalol
Sotalol has several well-recognized therapeutic applications in cardiology:
- Ventricular arrhythmias: Treatment of life-threatening ventricular tachycardia and ventricular fibrillation.
- Atrial fibrillation and atrial flutter: Maintenance of sinus rhythm in patients prone to recurrent episodes.
- Supraventricular tachycardia (SVT): Prevention of recurrent SVT episodes, improving quality of life for patients.
Off-Label Uses of Sotalol
Beyond its primary approvals, Sotalol is sometimes employed in scenarios where other antiarrhythmics are less effective or not tolerated:
- Management of pediatric arrhythmias, particularly in congenital heart disease cases.
- Adjunctive therapy for refractory atrial fibrillation when standard drugs prove insufficient.
- Investigational role in long QT syndromes and rare electrophysiological abnormalities.
Dosage and Administration Guidelines
Dosing with Sotalol must be carefully tailored to the individual. General recommendations include:
- Adults: Initiation at 80 mg twice daily, with titration based on therapeutic response and tolerance.
- Renal adjustments: Dosage must be modified according to renal function, as clearance is predominantly renal.
- Routes: Oral administration is standard for maintenance therapy, while intravenous use is reserved for acute arrhythmia control in hospitals.
- Monitoring: ECG and electrolyte levels should be checked during initiation and titration to minimize risks.
Administration in Special Populations
Elderly Patients
Older individuals often exhibit altered pharmacokinetics and increased susceptibility to adverse effects. They are particularly prone to QT prolongation and bradyarrhythmias, requiring cautious dose titration and vigilant monitoring.
Pregnant Women and Nursing Mothers
Sotalol crosses the placenta and may impact fetal development, with risks including growth restriction or neonatal bradycardia. During lactation, it can be secreted into breast milk, necessitating monitoring of infants for adverse cardiovascular effects.
Pediatric Use
In neonates and children, Sotalol has been used successfully, though evidence remains limited. Dosing requires meticulous calculation based on body weight, and frequent ECG monitoring is essential to avoid torsades de pointes.
Side Effects of Sotalol
Common Side Effects
Many patients tolerate Sotalol well, though common reactions can occur:
- Fatigue and dizziness
- Bradycardia and slowed pulse
- Gastrointestinal disturbances such as nausea and diarrhea
- Cold extremities and occasional sleep disturbances
Serious Adverse Reactions
In rare cases, severe outcomes necessitate immediate discontinuation and intervention:
- Torsades de pointes: A potentially fatal polymorphic ventricular tachycardia associated with prolonged QT interval.
- Severe hypotension and syncope: Leading to falls, fainting, or collapse.
- Bronchospasm: Especially in patients with asthma or chronic obstructive pulmonary disease.
These reactions underline the importance of careful selection, dosing, and continuous monitoring during Sotalol therapy.
Drug Interactions with Sotalol
Sotalol interacts with numerous pharmacological agents, and these interactions can significantly alter therapeutic outcomes. Careful attention to co-administered medications is essential to minimize risks.
Interactions with Other Antiarrhythmic Drugs
Concurrent use of antiarrhythmics such as amiodarone, quinidine, or procainamide can amplify the risk of severe ventricular arrhythmias. These combinations enhance QT prolongation, predisposing patients to torsades de pointes.
Interactions with QT-Prolonging Medications
- Antidepressants including tricyclics and selective serotonin reuptake inhibitors (SSRIs).
- Antipsychotic agents such as haloperidol, ziprasidone, or chlorpromazine.
- Macrolide antibiotics and certain fluoroquinolones.
These agents, when combined with Sotalol, may lead to additive electrophysiological effects, increasing arrhythmic risk.
Effect of Diuretics, Electrolyte Disturbances, and Digoxin
Hypokalemia and hypomagnesemia caused by loop or thiazide diuretics exacerbate Sotalol’s proarrhythmic potential. Co-administration with digoxin may potentiate bradycardia and conduction abnormalities, especially in patients with structural heart disease.
Alcohol and Food Interaction Considerations
Alcohol can intensify hypotensive effects and dizziness, while abrupt fluctuations in dietary potassium or magnesium intake may destabilize cardiac rhythm. Consistent nutritional patterns and avoidance of excess alcohol are strongly advised.
Contraindications to Sotalol Use
Certain conditions categorically preclude the use of Sotalol due to the high risk of adverse reactions:
- Known hypersensitivity to Sotalol or its excipients.
- Baseline prolonged QT interval or congenital long QT syndrome.
- Severe renal impairment leading to drug accumulation.
- Uncontrolled heart failure or cardiogenic shock.
- Asthma or severe chronic obstructive pulmonary disease, due to risk of bronchospasm.
Warnings and Important Precautions
Sotalol carries critical warnings that must be respected in all clinical settings:
- Black box warning: Proarrhythmic effects and the potential for torsades de pointes, particularly during therapy initiation.
- ECG monitoring: Mandatory during initiation or dose escalation to track QT interval changes.
- Electrolyte monitoring: Potassium and magnesium should be corrected and maintained within normal ranges.
- Avoid abrupt discontinuation: Sudden cessation may precipitate rebound arrhythmias or exacerbation of ischemic symptoms.
Careful Administration Considerations
Even in the absence of strict contraindications, caution is warranted in several patient populations:
- Diabetes: Beta-blockade may mask hypoglycemia symptoms, complicating glucose management.
- Thyroid disorders: May obscure clinical signs of hyperthyroidism or precipitate bradyarrhythmia in hypothyroidism.
- Renal impairment: As Sotalol is renally excreted, dose adjustments and close monitoring are imperative.
- Peripheral vascular disease: Risk of worsening circulation and exacerbation of symptoms such as claudication.
Overdosage of Sotalol
Signs and Symptoms
Overdose typically manifests as severe bradycardia, hypotension, cardiogenic shock, and dangerous arrhythmias. Central nervous system effects such as dizziness, fatigue, or fainting may also occur.
Emergency Treatment Strategies
- Administration of atropine or isoproterenol to counteract bradycardia.
- Intravenous fluids and vasopressors to restore blood pressure.
- Temporary cardiac pacing in refractory cases.
Role of Dialysis
Due to its renal clearance, hemodialysis can facilitate the removal of Sotalol in cases of severe toxicity, improving hemodynamic stability and reducing arrhythmic burden.
Storage and Handling Precautions
Maintaining the integrity of Sotalol requires adherence to proper storage protocols:
- Store at controlled room temperature, typically between 20°C to 25°C.
- Protect tablets from moisture, excessive heat, and direct sunlight.
- Keep in original packaging until administration to avoid degradation.
- Dispose of unused or expired medication through safe pharmaceutical disposal systems, avoiding environmental contamination.