1. Introduction
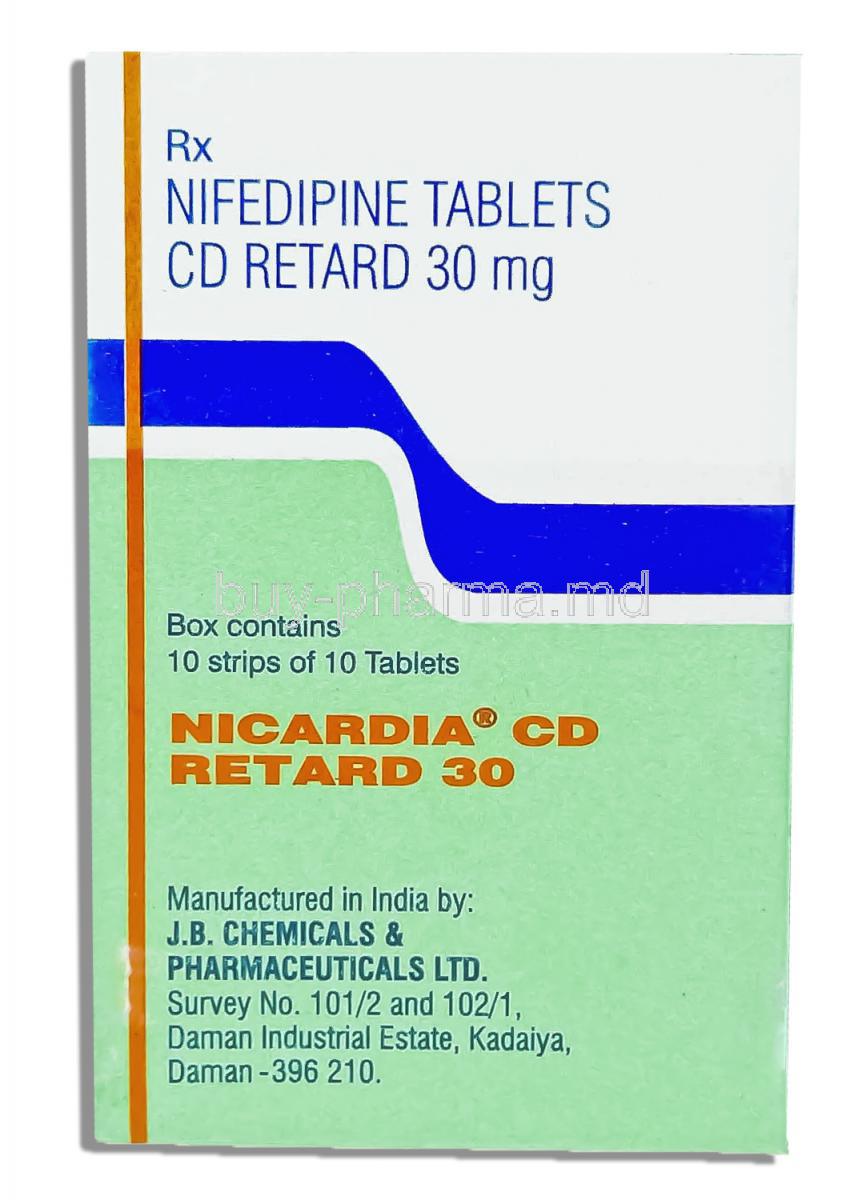
1.1 Overview of Nicardia Retard (Nifedipine)
Nicardia Retard is a sustained-release formulation of nifedipine, a well-established antihypertensive and antianginal medication. It delivers the active ingredient gradually, ensuring consistent plasma levels that support long-term cardiovascular control. This extended-release profile enhances therapeutic stability and minimizes abrupt fluctuations in blood pressure.
1.2 Therapeutic class: Calcium Channel Blocker (Dihydropyridine Class)
Nifedipine belongs to the dihydropyridine subclass of calcium channel blockers, a group known for its strong vasodilatory properties. These medicines target vascular smooth muscle to decrease arterial tension and improve circulatory efficiency.
1.3 Extended-release Formulation and Clinical Relevance
The retard (sustained-release) technology modulates drug absorption over many hours. This ensures:
- Stable pharmacokinetics
- Reduced frequency of dosing
- Lower incidence of reflex sympathetic activation
This controlled release makes Nicardia Retard particularly useful for chronic hypertension and angina management.
1.4 Key Benefits and Role in Cardiovascular Disease Management
Nicardia Retard supports long-term vascular health by optimizing arterial relaxation and improving oxygen delivery to myocardial tissue. It is widely utilized for:
- Reducing high blood pressure
- Preventing anginal episodes
- Enhancing coronary blood flow
2. Composition
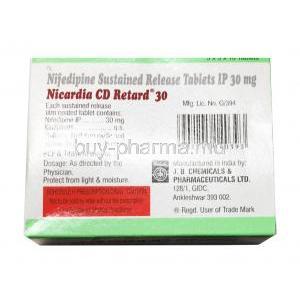
2.1 Active Ingredient: Nifedipine
Each sustained-release tablet contains nifedipine, a potent calcium influx inhibitor that primarily affects peripheral and coronary vasculature.
2.2 Mechanism-Supporting Excipients in Sustained-Release Tablets
The formulation incorporates specialized excipients such as hydrophilic polymers, microcrystalline cellulose, and osmotic agents. These components regulate dissolution, ensuring predictable and prolonged release of nifedipine.
2.3 Available Strengths and Formulations
Nicardia Retard is commonly available in 10 mg, 20 mg, and 30 mg sustained-release strengths, allowing individualized therapeutic tailoring.
2.4 Brand vs Generic Specifications
Both brand-name and generic variants deliver equivalent therapeutic effects. Generics follow stringent pharmacopeial standards to ensure bioequivalence, safety, and performance uniformity.
3. How Nicardia Retard Works
3.1 Mechanism of Action: Calcium Channel Blockade in Vascular Smooth Muscle
Nifedipine inhibits L-type calcium channels, reducing intracellular calcium within smooth muscle cells. The resultant vasodilation lowers systemic vascular resistance.
3.2 Reduction of Peripheral Vascular Resistance
By relaxing arteriolar smooth muscle, Nicardia Retard diminishes afterload. This leads to:
- Improved cardiac efficiency
- Lower blood pressure levels
- Reduced arterial stiffness
3.3 Improvement in Coronary Blood Flow
Coronary vasodilation enhances myocardial oxygenation, providing relief from ischemic discomfort and minimizing anginal attacks.
3.4 Impact on Cardiac Workload and Oxygen Demand
Reduced resistance decreases myocardial stress. The heart requires less oxygen, benefiting patients with chronic ischemic disease.
3.5 Pharmacokinetics of Sustained-Release Nifedipine
Extended-release nifedipine demonstrates gradual absorption, stable plasma concentrations, and prolonged therapeutic coverage—typically over 12 to 24 hours.
4. Uses of Nicardia Retard
4.1 Approved Uses
4.1.1 Hypertension (Primary and Secondary Hypertension)
Nicardia Retard is frequently prescribed to regulate elevated blood pressure, lowering the risk of stroke, heart attack, and renal complications.
4.1.2 Chronic Stable Angina
It alleviates chest discomfort associated with exertional ischemia by improving coronary perfusion.
4.1.3 Vasospastic (Prinzmetal’s) Angina
The medication is effective in mitigating coronary artery spasms, preventing episodes of rest angina.
4.2 Off-Label Uses
4.2.1 Raynaud’s Phenomenon
Nifedipine is commonly utilized to reduce vasospastic episodes in the extremities.
4.2.2 Preterm Labor Inhibition (Tocolytic Use)
The drug’s smooth muscle–relaxing effects may help delay premature uterine contractions.
4.2.3 Pulmonary Hypertension in Selected Cases
Some patients respond favorably to calcium channel blockade as part of specialized treatment regimens.
4.2.4 Hypertensive Emergency in Pregnancy (With Caution)
It may be administered in select obstetric hypertension scenarios under close supervision.
4.2.5 Esophageal Spasm Management
Nifedipine can reduce hypercontractility in esophageal smooth muscle.
4.3 Conditions Where Nicardia Retard Is Preferred Over Immediate-Release Nifedipine
The sustained-release form is favored because it:
- Provides smoother blood pressure control
- Reduces reflex tachycardia
- Has superior tolerability
5. Dosage and Administration
5.1 Standard Dosing Recommendations for Hypertension
Typical initial dosing begins at 20 mg once daily, adjusted according to therapeutic response.
5.2 Dosing for Chronic Stable Angina
Doses range from 20–40 mg daily to prevent anginal episodes and maintain coronary perfusion.
5.3 Dosing Adjustments for Vasospastic Angina
Some patients require higher maintenance dosing to prevent recurrent vasospasm.
5.4 Titration Schedule and Maximum Daily Dosage
The dose may be titrated gradually, with a usual maximum of 90 mg per day depending on clinical judgment.
5.5 Administration Instructions: Swallowing Whole vs Splitting Tablets
The sustained-release tablets must be swallowed whole. Splitting or crushing disrupts controlled-release kinetics.
5.6 Missed Dose Guidance
If a dose is missed, it should be taken promptly unless close to the next scheduled dose. Double dosing should be avoided.
5.7 Switching From Other Antihypertensives to Nicardia Retard
Transition must be gradual, allowing careful monitoring during dosage adjustments.
6. Important Precautions
6.1 Risk of Sudden Blood Pressure Drop
Excessive vasodilation may lead to symptomatic hypotension, necessitating cautious titration.
6.2 Avoiding Abrupt Discontinuation
Sudden cessation can trigger rebound hypertension or angina. Gradual tapering is advisable.
6.3 Interactions With Grapefruit and Citrus Bioflavonoids
Grapefruit inhibits CYP3A4, markedly increasing nifedipine concentration. Avoid concurrent ingestion.
6.4 Monitoring Heart Rate and Blood Pressure Regularly
Regular assessment ensures therapeutic safety and early detection of adverse reactions.
6.5 Driving and Operating Machinery Precautions
Dizziness or lightheadedness may impair alertness, particularly in early therapy.
6.6 Fluid Retention and Edema Monitoring
Peripheral edema is a common effect; clinical evaluation may be needed if swelling persists.
7. Contraindications
7.1 Hypersensitivity to Nifedipine
Any history of allergic reactions to nifedipine precludes use.
7.2 Advanced Aortic Stenosis
Marked vasodilation may exacerbate hemodynamic instability in this condition.
7.3 Cardiogenic Shock or Severe Heart Failure
Nifedipine can aggravate cardiac compromise in these severe states.
7.4 Unstable Angina (Specific Situations)
Immediate-release formulations may worsen instability; sustained-release should be used cautiously.
7.5 Concomitant Use With Potent CYP3A4 Inducers or Inhibitors
Certain agents may significantly alter nifedipine plasma levels.
8. Careful Administration (Use With Caution)
8.1 Patients With Liver Impairment
Reduced drug metabolism necessitates cautious dosing.
8.2 Patients With Severe Hypotension
Lower baseline blood pressure may increase the risk of syncope.
8.3 Heart Failure or Reduced Ejection Fraction
Patients require close supervision to prevent worsening symptoms.
8.4 Renal Impairment Considerations
Though primarily hepatic-metabolized, careful monitoring is advisable.
8.5 Concomitant Antihypertensives Increasing Risk of Hypotension
Additive hypotensive effects may occur with ACE inhibitors, ARBs, or diuretics.
8.6 Diabetic Patients and Autonomic Dysfunction
Autonomic instability may amplify blood pressure fluctuations.
8.7 Patients With Gastrointestinal Motility Issues
Delayed-release matrix relies on normal GI transit for optimal function.
9. Side Effects
9.1 Overview of Possible Adverse Reactions
Nicardia Retard is generally well tolerated but may cause systemic or localized reactions.
9.2 Vascular-Related Effects
9.2.1 Peripheral Edema
A frequent effect caused by pre-capillary vasodilation.
9.2.2 Hypotension
Marked falls in blood pressure may occur at higher doses.
9.2.3 Reflex Tachycardia
The sympathetic system may respond to vasodilation by increasing heart rate.
9.3 Central Nervous System Effects
9.3.1 Dizziness and Headache
These are common early-treatment manifestations.
9.3.2 Fatigue or Lethargy
Some individuals may experience reduced physical vigor.
9.4 Gastrointestinal Effects
9.4.1 Nausea
Mild gastric upset occurs in some patients.
9.4.2 Constipation
Slowed transit time may lead to bowel changes.
9.5 Dermatological and Allergic Reactions
Rare but possible reactions include rash, pruritus, and urticaria.
9.6 Long-Term Safety Profile
Long-term use is generally safe with proper monitoring and dose adjustments.
10. Common Side Effects
10.1 Ankle and Lower-Leg Swelling
One of the hallmark effects of dihydropyridine therapy.
10.2 Flushing and Warmth Sensation
Transient vasodilation may lead to facial warmth.
10.3 Headache
Often improves as the body adapts to treatment.
10.4 Palpitations
Occasional awareness of heartbeat due to reflex tachycardia.
10.5 Lightheadedness
More noticeable when rising from a seated position.
10.6 Mild Gastrointestinal Discomfort
Typically self-limiting and manageable.
11. Drug Interactions
11.1 CYP3A4 Inhibitors (e.g., Azole Antifungals, Macrolides)
CYP3A4 inhibitors markedly elevate plasma concentrations of nifedipine. This occurs because the metabolic degradation of the drug slows dramatically. As a result, patients may experience exaggerated vasodilatory effects. These may include dizziness, profound hypotension, or peripheral edema.
- Ketoconazole and itraconazole can significantly amplify drug levels.
- Macrolides such as erythromycin may induce hypertensive instability due to excess circulating drug.
11.2 CYP3A4 Inducers (e.g., Rifampin, Carbamazepine, Phenytoin)
Potent enzyme inducers accelerate the metabolic clearance of nifedipine, often rendering therapy less effective. Blood pressure may rise unpredictably, and anginal control may deteriorate.
- Rifampin can virtually eliminate therapeutic efficacy.
- Carbamazepine and phenytoin reduce systemic exposure, necessitating alternative regimens.
11.3 Antihypertensive Drugs Leading to Additive Effects
Combination therapy with other antihypertensive agents can produce cumulative blood pressure reduction. While sometimes desirable, excessive hypotension may develop if adjustments are not carefully calibrated.
- ACE inhibitors
- ARBs
- Diuretics
11.4 Beta-Blockers: Combined Cardiovascular Impact
Concurrent use with beta-blockers alters hemodynamics. The synergistic reduction in blood pressure may be accompanied by reflex tachycardia suppression, creating complex cardiovascular dynamics. Patients should be observed for bradycardia or conduction irregularities.
11.5 Grapefruit Juice Metabolism Interaction
Grapefruit juice inhibits intestinal CYP3A4, causing elevated nifedipine bioavailability. This can precipitate intensified pharmacological effects. Avoiding grapefruit products ensures stable therapeutic exposure.
11.6 Immunosuppressants (e.g., Tacrolimus) Requiring Dose Modifications
Immunosuppressants dependent on CYP3A4 metabolism may accumulate when used with nifedipine. Tacrolimus levels can rise precipitously, raising the risk of neurotoxicity or nephrotoxicity.
- Regular monitoring of tacrolimus trough levels is essential.
- Dose modifications may be mandatory.
11.7 Antiretrovirals Interaction Considerations
Several antiretroviral medications modulate CYP3A4 functionality, complicating therapeutic stability. Protease inhibitors often inhibit metabolism, while non-nucleoside reverse transcriptase inhibitors may accelerate clearance. The interaction landscape requires precise oversight.
12. Administration to Specific Populations
12.1 Elderly Patients
12.1.1 Increased Sensitivity to Blood Pressure Lowering
Older adults often exhibit amplified sensitivity to vasodilatory agents. Even standard doses may provoke symptomatic hypotension. This predisposition results from decreased vascular elasticity and altered autonomic responses.
12.1.2 Dose Adjustments and Monitoring Recommendations
Dosing should begin conservatively. Slow titration prevents excessive hypotension. Routine assessments of pulse, blood pressure, and dizziness episodes are recommended.
12.2 Pregnant Women and Nursing Mothers
12.2.1 Safety Profile in Pregnancy
Nifedipine has been utilized during pregnancy under specific clinical scenarios. Although generally considered low risk, therapy should be supervised by experienced clinicians.
12.2.2 Use in Preeclampsia and Gestational Hypertension
The drug may be deployed to control elevated blood pressure in pregnancy-related hypertensive syndromes. Its vasodilatory action assists in stabilizing maternal hemodynamics.
12.2.3 Transfer Into Breast Milk and Infant Safety
Minimal amounts of nifedipine pass into breast milk. Adverse infant effects are uncommon, yet monitoring is prudent, particularly in neonates with low birth weight.
12.3 Children
12.3.1 Safety and Efficacy Evidence
Pediatric data remain limited. The drug is not routinely used in young children unless guided by a specialist.
12.3.2 Pediatric Hypertension Considerations
Management of pediatric hypertension requires careful assessment. If nifedipine is selected, dosing must be individualized with exceptional vigilance.
12.3.3 Specialist-Guided Dosing Only
Pediatric administration must be supervised by clinicians with expertise in pediatric cardiovascular medicine.
13. Overdosage
13.1 Symptoms of Overdose
13.1.1 Severe Hypotension
Profound vasodilation leads to dangerously low blood pressure. Patients may collapse or experience syncope.
13.1.2 Shock and Cardiac Complications
Circulatory shock may ensue, accompanied by reduced organ perfusion. Arrhythmias or myocardial ischemia may develop.
13.1.3 Metabolic Acidosis
Severe overdose can impair cellular metabolism, resulting in metabolic acidosis—marked by rapid breathing and confusion.
13.2 Emergency Management
13.2.1 Gastric Lavage and Activated Charcoal
Prompt gastric decontamination may reduce absorption. Activated charcoal can bind residual drug within the gastrointestinal tract.
13.2.2 Intravenous Fluids and Vasopressors
Circulatory support is critical. IV fluids restore volume, while vasopressors counter life-threatening hypotension.
13.2.3 Continuous Cardiovascular Monitoring
Ongoing electrocardiographic and hemodynamic monitoring ensures timely detection of cardiac complications.
13.3 Prognosis After Overdose
Recovery depends on dose magnitude, rapidity of intervention, and baseline patient health. With aggressive supportive care, full recovery is achievable.
14. Storage
14.1 Recommended Storage Temperature
Tablets should be stored at controlled room temperature, typically between 20°C and 25°C. Temperature stability preserves potency.
14.2 Protecting Tablets From Moisture and Light
Moisture can compromise the sustained-release matrix. Tablets must remain in tightly sealed packaging and protected from direct light exposure.
14.3 Safe Storage Away From Children and Pets
Accidental ingestion can provoke severe hypotension. Medications should always be kept in secure, inaccessible locations.
14.4 Shelf-Life and Expiration Guidance
The expiration date ensures maximal efficacy. Tablets should not be used beyond their printed shelf-life.
15. Handling Precautions
15.1 Tablet Integrity and Preventing Crushing
Sustained-release tablets must not be split, crushed, or chewed. Altering their structure disrupts controlled drug release and may cause dangerous hemodynamic effects.
15.2 Safe Handling for Caregivers
Caregivers should handle tablets with clean, dry hands. Contact with moisture may weaken the tablet matrix.
15.3 Disposal of Unused or Expired Medication
Unused medication should be discarded responsibly. Many regions recommend pharmacy take-back programs to avoid environmental contamination.
15.4 Guidance for Pharmacists and Healthcare Institutions
Pharmacists must ensure proper storage, labeling, and counseling. Healthcare facilities should maintain adherence to regulatory standards for medication management and disposal.