1. Introduction
Atarax, known generically as Hydroxyzine Hydrochloride, is a multifaceted medication belonging to the class of first-generation antihistamines. It exhibits potent sedative, anxiolytic, and antipruritic properties, making it a versatile agent in both psychiatry and allergy management. Originally developed in the mid-20th century, Hydroxyzine was one of the first antihistamines recognized for its ability to cross the blood–brain barrier and influence the central nervous system. Hydroxyzine gained prominence for its dual efficacy in treating allergic reactions and anxiety-related disorders. Today, it is available globally under numerous brand names—such as Atarax, Vistaril, and Ucerax—with formulations tailored to clinical needs. While Hydroxyzine HCl (Hydrochloride) is primarily used in oral and injectable forms, Hydroxyzine Pamoate is more commonly reserved for encapsulated preparations with a slower onset and prolonged effect. Key distinctions between Hydroxyzine HCl and Pamoate salts lie in their pharmacokinetic behavior: the HCl salt is faster-acting, suitable for acute symptoms, whereas the Pamoate variant offers sustained sedative effects ideal for chronic anxiety management. ---
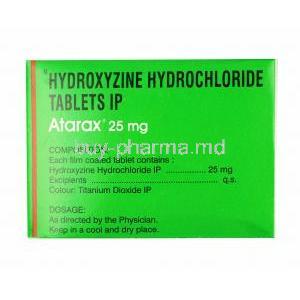
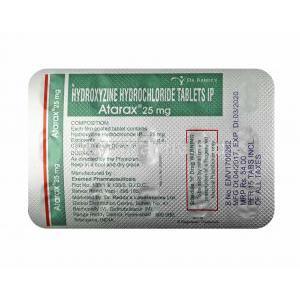
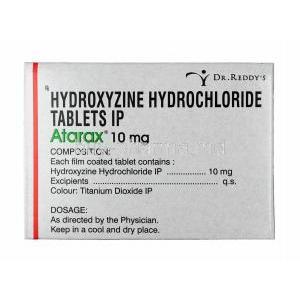
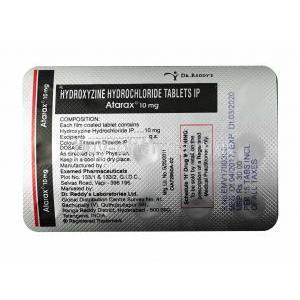
2. Composition and Formulation
The active component of Atarax is **Hydroxyzine Hydrochloride**, a piperazine derivative with the molecular formula C21H27ClN2O2·HCl. This compound functions as a potent antagonist of peripheral H1 histamine receptors and a modulator of central neuronal activity. **Available forms include:** * Tablets: 10 mg, 25 mg, and 50 mg strengths * Oral syrup: for pediatric or geriatric administration * Injectable formulations: typically for hospital-based use **Inactive ingredients** often comprise lactose, magnesium stearate, microcrystalline cellulose, and coloring agents depending on manufacturer specifications. **Pharmacokinetics:** Hydroxyzine is rapidly absorbed after oral administration, with onset of action within 15–30 minutes. It undergoes hepatic metabolism primarily via CYP3A4/5 to form cetirizine (its active metabolite). Elimination occurs mainly through renal excretion, with a half-life averaging 20–25 hours in adults. ---
3. Mechanism of Action (How Atarax Works)
Hydroxyzine operates primarily by **blocking H1 histamine receptors**, reducing the effects of histamine on smooth muscle and capillaries, which alleviates itching and allergic symptoms. Beyond its antihistaminic action, Atarax exerts **central nervous system depressant effects**, mediated through suppression of subcortical activity, producing mild sedation and anxiolysis. **Additional mechanisms include:** * **Antiemetic activity:** inhibition of chemoreceptor trigger zones in the medulla oblongata. * **Antipruritic effect:** suppression of histamine-mediated sensory nerve responses in the skin. * **Serotonergic and muscarinic modulation:** contributing to mood stabilization and antiemetic properties. The onset of therapeutic relief is rapid, while the duration of effect generally spans 4–6 hours, with residual anxiolytic influence extending longer in some individuals. ---
4. Therapeutic Uses of Atarax
Atarax is employed across multiple medical disciplines due to its **broad pharmacological profile**. **Primary Indications:** * **Allergic disorders:** relief from urticaria, pruritus, contact dermatitis, and seasonal allergic rhinitis. * **Anxiety and tension:** adjunctive therapy for short-term management of generalized anxiety disorder. * **Preoperative and postoperative sedation:** as an adjunct in anesthesia to calm patients and reduce nausea. * **Nausea and vomiting control:** prevention of motion sickness or postoperative nausea. Its therapeutic value is well-documented through clinical studies confirming efficacy in both dermatologic and psychoneurotic disorders. ---
5. Off-Label and Experimental Uses
Hydroxyzine’s pharmacologic versatility has led to numerous **off-label applications**, supported by anecdotal and clinical data. **Off-label indications include:** * **Insomnia management:** as a non-habit-forming sleep aid due to sedative and anxiolytic effects. * **Chronic pain and fibromyalgia:** adjuvant use for reducing somatic anxiety and muscle tension. * **Withdrawal therapy:** mitigation of anxiety and irritability in opioid or alcohol detoxification. * **Psychodermatologic disorders:** to address pruritus and emotional distress linked to chronic eczema. * **Palliative care:** reduction of agitation and restlessness in terminally ill patients. These expanded roles underscore hydroxyzine’s adaptability across clinical domains. ---
6. Dosage and Administration
**Standard Adult Dosing:** * For anxiety: 50 mg to 100 mg daily in divided doses. * For pruritus and allergies: 25 mg taken three to four times daily. **Pediatric Dosage:** * For allergic conditions: 0.6 mg/kg every 8 hours or as directed by a physician. **Dose Adjustments:** * In hepatic or renal impairment, lower doses are advised to prevent accumulation. * Elderly patients should start at half the usual adult dose due to prolonged elimination. **Administration Guidelines:** * May be taken with or without food. * Evening doses can minimize daytime drowsiness. * Gradual dose tapering is recommended to avoid rebound symptoms. The duration of therapy depends on the underlying condition and patient tolerance, typically ranging from several days to a few weeks. ---
7. Side Effects and Adverse Reactions
Hydroxyzine generally demonstrates an excellent safety record, though certain side effects are common due to its CNS and anticholinergic actions. Reactions may vary in intensity based on individual susceptibility and dosage.
7.1 Common Side Effects
- Drowsiness or somnolence - Fatigue and dizziness - Dry mouth or mild thirst sensation - Gastrointestinal upset such as nausea or constipation - Blurred vision and mild cognitive confusion in sensitive individuals
7.2 Serious Adverse Effects
- **QT prolongation** and risk of arrhythmia, particularly with co-administered cardiac drugs - **Severe hypersensitivity or angioedema** requiring emergency treatment - **CNS depression**, especially in concurrent use with alcohol or sedatives - **Urinary retention** and ocular disturbances in patients with prostatic hypertrophy or glaucoma Immediate medical intervention is warranted in the event of palpitations, syncope, or swelling of the face and throat. ---
8. Drug Interactions
Atarax may interact with multiple pharmacologic agents due to its sedative and anticholinergic profile. **Major interaction categories:** * **CNS depressants:** alcohol, benzodiazepines, and opioids intensify sedation. * **Anticholinergic drugs:** additive effects leading to increased dryness, constipation, or urinary retention. * **QT-prolonging medications:** macrolide antibiotics, antiarrhythmics, and certain antipsychotics heighten cardiac risk. * **CYP3A4 inhibitors:** may delay hydroxyzine metabolism and prolong effects. Combination therapy should be approached with clinical discretion, and patients should be advised to avoid alcohol during treatment. ---
9. Warnings and Important Precautions
* Avoid operating heavy machinery or driving until individual response is known. * Prolonged use should be limited to short therapeutic courses to prevent tolerance. * **Cardiac caution:** patients with a history of arrhythmia, bradycardia, or electrolyte imbalance should undergo ECG evaluation. * **Hepatic or renal impairment:** periodic monitoring of function is advised. * **Glaucoma and urinary retention:** risk of symptom exacerbation due to anticholinergic properties. * Regular re-evaluation of treatment necessity is essential for long-term users. Atarax, when used judiciously under medical supervision, remains a cornerstone in the management of allergic, psychoneurotic, and somatic tension disorders—balancing efficacy with safety through careful administration and monitoring.
10. Contraindications
Atarax (Hydroxyzine Hydrochloride) should not be administered in specific clinical situations where the potential for harm outweighs any therapeutic benefit. Understanding these contraindications is vital to ensure patient safety and effective pharmacologic stewardship. * **Hypersensitivity to Hydroxyzine or Related Compounds:** Individuals with known allergic reactions to hydroxyzine, cetirizine, or other piperazine derivatives must avoid its use due to the risk of cross-reactivity leading to rash, bronchospasm, or anaphylaxis. * **Early Pregnancy (Especially First Trimester):** Hydroxyzine has been associated with potential teratogenic effects in animal studies. Its use during the first trimester is contraindicated because of potential interference with fetal neurodevelopment and the risk of congenital anomalies. * **Severe Cardiac Disorders and Known QT Prolongation:** Patients with existing arrhythmias, prolonged QT interval, or those on concomitant QT-prolonging drugs face an increased risk of torsades de pointes or cardiac arrest. * **Porphyria or Severe CNS Depression:** Hydroxyzine may exacerbate porphyric symptoms and potentiate CNS depression, particularly in patients concurrently using sedatives, barbiturates, or alcohol. ---
11. Careful Administration and Monitoring
Prudent management and surveillance enhance the therapeutic efficacy of Atarax while mitigating risks. Continuous observation and adjustment are critical for patients on prolonged or high-dose therapy. * **Regular Assessment of Sedation and Alertness Levels:** Monitoring for drowsiness, cognitive slowing, or excessive sedation is essential, especially in patients operating machinery or performing complex tasks. * **Liver and Kidney Function Monitoring During Long-Term Therapy:** Periodic hepatic and renal assessments are recommended since hydroxyzine is metabolized hepatically and excreted renally. Dose adjustments should be made in organ impairment. * **ECG Monitoring for At-Risk Patients:** Patients with pre-existing cardiac conditions should undergo periodic ECG evaluation to detect potential QT prolongation. * **Gradual Dose Reduction When Discontinuing Therapy:** To prevent withdrawal symptoms such as insomnia, irritability, or rebound anxiety, tapering the dose rather than abrupt cessation is advisable. ---
12. Use in Special Populations
12.1 Administration to Elderly Patients
Elderly patients exhibit altered pharmacodynamics and reduced metabolic clearance, making them particularly sensitive to hydroxyzine’s sedative and anticholinergic effects. * **Reduced Drug Clearance and Enhanced Sedative Effect:** Age-related hepatic and renal decline leads to accumulation and prolonged sedation. * **Increased Risk of Confusion and Falls:** Cognitive impairment, dizziness, and orthostatic hypotension may heighten fall risk in frail individuals. * **Recommended Dose Adjustment and Monitoring:** Initiate therapy at the lowest effective dose (typically half the adult dose) with close clinical monitoring for tolerance.
12.2 Administration to Pregnant Women and Nursing Mothers
Caution is warranted in pregnancy and lactation, as hydroxyzine can cross the placental barrier and may be excreted in breast milk. * **Safety Concerns During Pregnancy and Lactation:** Although no large-scale human studies confirm teratogenicity, animal models show embryotoxicity, particularly during organogenesis. * **Potential Fetal Risk and Neonatal Withdrawal Symptoms:** Prolonged maternal use near term may cause neonatal hypotonia, CNS depression, or withdrawal reactions. * **Alternatives and Guidelines for Breastfeeding:** Prefer antihistamines with established safety profiles during pregnancy (e.g., loratadine). Nursing mothers should avoid Atarax or discontinue breastfeeding if therapy is essential.
12.3 Administration to Children
Hydroxyzine is approved for pediatric use in anxiety and allergic conditions but requires careful dose calibration. * **Age-Appropriate Dosing:** Typically 0.6 mg/kg every 8 hours for allergic manifestations; individualized under medical supervision. * **Monitoring for Paradoxical Excitation:** Some children may develop hyperactivity, irritability, or insomnia rather than sedation. * **Use Limitations in Infants and Toddlers:** Contraindicated in neonates and infants under 6 months due to immature metabolic pathways and enhanced CNS susceptibility. ---
13. Overdosage and Emergency Management
Exceeding recommended doses of Atarax can precipitate severe toxic manifestations requiring urgent medical attention. **Symptoms of Overdose:** * Extreme drowsiness or stupor * Tremors, convulsions, or seizures * Hypotension, cardiac arrhythmias, or respiratory depression **Immediate Management:** * Perform **gastric lavage** or administer activated charcoal if ingestion was recent. * Ensure **supportive care** with airway maintenance and oxygenation. * Initiate **ECG monitoring** to detect QT prolongation or arrhythmia. **Antidotal Considerations:** * There is no specific antidote for hydroxyzine toxicity. * Symptomatic treatment with intravenous fluids, benzodiazepines for seizures, and vasopressors for hypotension is indicated. * Continuous observation for 24–48 hours post-crisis is recommended. ---
14. Handling and Storage Precautions
Proper storage preserves potency and ensures safety. * **Recommended Storage Temperature:** Maintain at 15–25°C in a dry environment away from direct sunlight and humidity. * **Protection from Moisture and Light:** Use original blister packs or amber bottles to prevent degradation. * **Shelf Life and Disposal:** Follow manufacturer’s expiry guidelines; dispose of unused tablets through pharmaceutical take-back programs. * **Safe Handling:** Keep out of reach of children and pets to prevent accidental ingestion and potential toxicity. ---
15. Patient Education and Key Takeaways
Educating patients on correct usage enhances safety and adherence. * **Adhering to Prescribed Dosage and Timing:** Never increase or skip doses without professional guidance. * **Avoiding Alcohol and Sedative Combinations:** Concurrent use may potentiate CNS depression and impair cognition. * **Recognizing Signs of Adverse Effects or Overdose:** Persistent dizziness, palpitations, or confusion warrant prompt medical evaluation. * **When to Seek Medical Attention:** Contact a healthcare provider immediately in cases of severe drowsiness, allergic reaction, or cardiac irregularities. Consistent medical supervision, adherence to dosing protocols, and awareness of contraindications ensure that Atarax therapy remains effective, safe, and well-tolerated across diverse patient populations.