Introduction
Eslicarbazepine acetate is an antiseizure medicine engineered to stabilize aberrant cortical excitability. It serves patients with focal (partial-onset) seizures by attenuating electrical paroxysms that disrupt daily function. Concise dosing, predictable kinetics, and once-daily administration contribute to clinical practicality.
- Designed for long-term seizure control
- Structurally related to carbamazepine and oxcarbazepine, yet pharmacologically streamlined
- Suitable as monotherapy or as an adjunct in appropriately selected patients
Overview of Eslicarbazepine Acetate
Eslicarbazepine acetate is a prodrug rapidly converted to its active metabolite, eslicarbazepine, after oral administration. The agent targets neuronal sodium channels to reduce repetitive firing, thereby diminishing seizure propensity.
Historical Background and Approval Timeline
Conceptualized to refine the tolerability profile of first-generation dibenzazepine derivatives, development advanced through comparative trials in focal epilepsy. Regulatory authorizations were granted across multiple regions in the late 2000s and 2010s for adult focal seizures, with subsequent label expansions into pediatric cohorts in certain jurisdictions.
- Origin: rational modification of dibenzazepine scaffold
- Trajectory: adult approval → pediatric data accretion → broader real-world use
- Ongoing: pharmacovigilance registries tracking hyponatremia, dermatologic reactions, and neuropsychiatric signals
Classification as an Antiepileptic Drug (AED)
Pharmacologic class: voltage-gated sodium channel modulator. Clinical class: antiseizure medication for focal epilepsy. Therapeutic aim: reduce seizure frequency and intensity without compromising cognition or systemic safety.
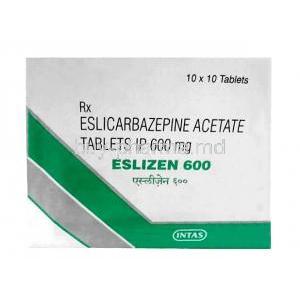
Composition and Formulations
Active Ingredient: Eslicarbazepine Acetate
The active moiety delivered systemically is eslicarbazepine, formed via rapid first-pass hydrolysis. Minor metabolites include (R)-licarbazepine and oxcarbazepine in trace amounts.
Available Dosage Forms (Tablets, Oral Suspension)
Manufactured as film-coated tablets and, in some markets, a measurable oral suspension to facilitate pediatric and dysphagic use. Once-daily dosing simplifies adherence.
- Strengths commonly span low to high milligram ranges for titration flexibility
- Scored tablets may support dose adjustments where approved
Inactive Components and Excipients
Typical excipients include microcrystalline cellulose, starches, lactose or alternative fillers, disintegrants, and film-coating polymers. Verify product-specific excipient lists for sensitivities (e.g., lactose intolerance, dye reactions).
Mechanism of Action: How Eslicarbazepine Works
Influence on Voltage-Gated Sodium Channels
Eslicarbazepine preferentially enhances slow inactivation of voltage-gated sodium channels (Nav), stabilizing neuronal membranes and suppressing high-frequency discharges that precipitate focal seizures.
Reduction of Neuronal Hyperexcitability
By curbing pathologic depolarization, the drug diminishes the spread of epileptiform activity across cortical networks. This translates into fewer clinical events and attenuated interictal spikes.
Comparison with Related Drugs (Carbamazepine, Oxcarbazepine)
- Carbamazepine: potent but enzyme-inducing; broader interaction burden
- Oxcarbazepine: similar scaffold; higher propensity for hyponatremia in some cohorts
- Eslicarbazepine: slow-inactivation bias and once-daily kinetics; interaction profile may be more manageable
Clinical selection weighs prior response, comorbidities, interaction risk, and electrolyte vulnerability.
Approved Medical Uses
Monotherapy for Partial-Onset Seizures in Adults
Indicated as initial or conversion therapy in adults with focal seizures, with or without secondary generalization. Conversion from other sodium channel agents is common in practice.
Adjunctive Therapy for Partial-Onset Seizures in Adults and Children
Used alongside other AEDs when monotherapy proves inadequate. Synergy with non-sodium channel agents may enhance seizure reduction while mitigating additive adverse effects.
Indications in Specific Seizure Subtypes
Most robust data exist for focal seizures with or without secondary generalization. Use in generalized epilepsies should be individualized and evidence-guided.
Off-Label Uses
Management of Trigeminal Neuralgia
In refractory cases or intolerance to first-line agents, eslicarbazepine may be considered to dampen paroxysmal facial pain via sodium channel modulation.
Investigational Use in Bipolar Disorder
Exploratory studies evaluate mood-stabilizing potential given mechanistic kinship to carbamazepine. Evidence remains preliminary; psychiatric use should be research-aligned.
Potential Role in Neuropathic Pain Syndromes
Pathways implicated in ectopic neuronal firing suggest possible benefit; formal evidence is evolving and patient selection is key.
Dosage and Administration
Recommended Starting Dosage for Adults
Initiate once daily at a low or intermediate dose, then titrate based on efficacy and tolerability. Evening dosing may mitigate early dizziness or somnolence.
Titration Schedules for Seizure Control
- Increase at weekly or biweekly intervals
- Aim for the minimal effective dose that sustains seizure reduction
- Adjust more gradually in patients prone to hyponatremia or CNS effects
Pediatric Dosing Guidelines
Weight-normalized regimens are utilized where approved. Liquid formulations enable precise titration in younger children.
Adjustments for Renal and Hepatic Impairment
- Renal: dose reductions or extended titration intervals when creatinine clearance is reduced
- Hepatic: caution in moderate impairment; avoid in severe impairment per local labeling
Administration Tips (With or Without Food, Tablet Swallowing vs. Suspension)
May be taken with or without food. Swallow tablets whole unless the product information permits splitting. Shake suspensions thoroughly; use a calibrated measuring device.
Side Effects of Eslicarbazepine Acetate
Common Side Effects
Dizziness and Somnolence
Often transient during titration. Slower up-titration or evening dosing can improve tolerability.
Nausea, Vomiting, Abdominal Discomfort
Generally mild and self-limiting. Administration with food may help sensitive patients.
Headache and Fatigue
Report patterns that persist beyond the titration phase. Consider dose adjustment if functional impairment occurs.
Blurred Vision and Diplopia
Visual disturbances can accompany CNS effects; avoid driving or operating machinery until stabilized.
Less Common but Serious Side Effects
Hyponatremia and Electrolyte Imbalance
Monitor serum sodium, especially in the elderly, patients on diuretics, and those with prior oxcarbazepine-related hyponatremia. Symptoms include confusion, gait instability, and seizures.
Hepatotoxicity and Elevated Liver Enzymes
Periodically assess hepatic transaminases in symptomatic patients. Discontinue if significant liver injury is suspected.
Dermatological Reactions (Stevens–Johnson Syndrome, Rash)
Rash warrants prompt evaluation. Severe mucocutaneous reactions necessitate immediate cessation and urgent care.
Suicidal Ideation and Psychiatric Effects
All AEDs carry a class warning for suicidality. Screen for mood changes, anxiety, agitation, or emergent depression—particularly during initiation and dose changes.
Warnings and Important Precautions
Risk of Suicidal Behavior and Monitoring Mental Health
Like many antiepileptic drugs, eslicarbazepine acetate carries a risk of increasing suicidal thoughts or behaviors. Patients should be observed for any sudden mood changes, anxiety, agitation, or emerging depressive symptoms. Healthcare providers may recommend regular mental health evaluations, particularly during the first few months of therapy or after dosage adjustments.
- Monitor closely for signs of self-harm or mood instability
- Family members and caregivers should be informed to observe behavioral changes
- Prompt reporting of psychiatric disturbances is essential
Danger of Abrupt Discontinuation
Sudden cessation of therapy can precipitate breakthrough seizures or status epilepticus, a medical emergency. Tapering the dose gradually under medical supervision is advised to reduce rebound seizure risk.
Seizure Exacerbation in Certain Cases
Although designed to control seizures, in rare circumstances eslicarbazepine may paradoxically worsen seizure activity. If seizure frequency or severity increases, clinical reassessment is mandatory.
Caution with Driving or Operating Machinery
Dizziness, blurred vision, and somnolence may impair psychomotor performance. Until stability of response is confirmed, patients should avoid driving, operating heavy machinery, or engaging in hazardous activities.
Contraindications
Hypersensitivity to Eslicarbazepine or Related Drugs
Patients with known allergic reactions to eslicarbazepine, carbamazepine, or oxcarbazepine should not use this medication due to the high likelihood of cross-reactivity.
Severe Hepatic Impairment
Administration is contraindicated in individuals with severe hepatic dysfunction as metabolism and clearance may be compromised, leading to toxicity.
Known History of Allergic Reaction to Carbamazepine or Oxcarbazepine
Cross-hypersensitivity is well documented. Severe cutaneous or systemic allergic reactions with related agents prohibit the use of eslicarbazepine.
Careful Administration and Special Populations
Administration to Elderly Patients
Pharmacokinetic Considerations
Aging alters renal clearance, increasing drug exposure. Dose adjustments and slower titration schedules may be required to reduce adverse reactions.
Fall Risk and Monitoring Dizziness
Orthostatic dizziness, imbalance, and sedation elevate fall risk. Regular assessment of gait and balance is prudent in geriatric patients.
Administration to Pregnant Women and Nursing Mothers
Pregnancy Category and Fetal Risk Data
Data on eslicarbazepine use during pregnancy remain limited. Animal studies indicate potential teratogenicity, though human evidence is not definitive.
Teratogenicity Concerns and Seizure Control Balance
The clinician must weigh fetal risks against maternal seizure control, as uncontrolled seizures may endanger both mother and fetus.
Excretion in Breast Milk and Breastfeeding Precautions
Eslicarbazepine is excreted in human milk. Breastfeeding infants should be monitored for sedation, irritability, or feeding difficulties if maternal therapy is continued.
Administration to Children
Safety Profile in Pediatric Epilepsy
Clinical trials support efficacy and safety in pediatric epilepsy, though younger children may be more sensitive to adverse reactions.
Approved Age Ranges
Approval varies by jurisdiction, with many regions permitting use from age six and above as adjunctive therapy.
Dosage Considerations in Children and Adolescents
Dosing is typically weight-based. Careful titration helps minimize somnolence, dizziness, and gastrointestinal effects.
Drug Interactions
Interaction with CYP3A4 Inducers and Inhibitors
Strong inducers may lower eslicarbazepine levels, reducing efficacy, while inhibitors can elevate concentrations, increasing toxicity risk.
Effects on Hormonal Contraceptives
Eslicarbazepine may reduce the effectiveness of oral contraceptives. Alternative or backup contraceptive methods are recommended.
Interaction with Warfarin, Statins, and Antidiabetic Drugs
Co-administration can alter plasma concentrations of these drugs, necessitating dosage adjustments and closer clinical monitoring.
Potential Additive Effects with Other Antiepileptics
Combination with other sodium channel blockers may increase CNS side effects, whereas pairing with complementary mechanisms may improve seizure control.
Overdosage and Emergency Management
Clinical Manifestations of Overdose
Symptoms may include pronounced dizziness, nausea, vomiting, somnolence, ataxia, hyponatremia, and cardiac conduction disturbances.
Supportive Treatment and Symptomatic Management
There is no specific antidote. Management includes airway protection, gastric decontamination if recent ingestion, and supportive care for CNS and cardiovascular symptoms.
Monitoring Electrolyte Levels and Cardiac Rhythm
Continuous cardiac monitoring and frequent electrolyte checks are essential. Severe hyponatremia requires corrective interventions.
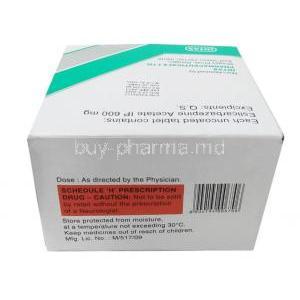
Storage and Handling Precautions
Recommended Storage Temperature and Conditions
Store at controlled room temperature, typically 20–25°C (68–77°F). Protect from moisture and direct light.
Shelf Life and Stability Considerations
Use within the expiration date indicated on the packaging. Reconstituted suspensions should be consumed within the specified timeframe to ensure stability.
Safe Handling Instructions for Healthcare Professionals
Wear protective gloves when handling crushed or broken tablets. Avoid inhalation of powder or contact with skin and mucous membranes.
Disposal Guidelines for Unused Medication
Dispose of unused or expired medication according to local regulations. Do not flush into wastewater; return to designated pharmaceutical disposal programs when available.
Eslicarbazepine Acetate FAQ
- What is eslicarbazepine acetate used for?
- Is eslicarbazepine acetate better than carbamazepine?
- Is eslicarbazepine a mood stabilizer?
- When to take eslicarbazepine?
- What should I avoid while taking eslicarbazepine?
- Is eslicarbazepine safe for elderly people?
- Is eslicarbazepine hazardous?
- What is eslicarbazepine 400 mg used for?
- What are the side effects of taking eslicarbazepine?
- What are the blood levels for eslicarbazepine?
- How effective is eslicarbazepine?
- How does eslicarbazepine work?
- What should I avoid while taking eslicarbazepine?
What is eslicarbazepine acetate used for?
Eslicarbazepine is utilized either on its own or in combination with other medications to manage partial seizures (convulsions) in the treatment of epilepsy.
Is eslicarbazepine acetate better than carbamazepine?
Eslicarbazepine acetate is a less potent enzyme inducer compared to carbamazepine, which lowers the potential for drug interactions. Eslicarbazepine acetate is also less prone to causing hyponatremia than both carbamazepine and oxcarbamazepine.
Is eslicarbazepine a mood stabilizer?
Eslicarbazepine (ESL) is thought to work similarly to an active metabolite of the widely used carbamazepine (CBZ). Carbamazepine is employed as a psychotropic medication to aid in various psychiatric conditions, including mood disorders, aggression, and anxiety.
When to take eslicarbazepine?
Same time as other medications
What should I avoid while taking eslicarbazepine?
- Avoid driving, operating machinery, or participating in potentially dangerous activities that require mental alertness and motor coordination
Is eslicarbazepine safe for elderly people?
No specific safety concerns were noted regarding the use of eslicarbazepine acetate (ESL) for treating focal seizures in elderly patients
Is eslicarbazepine hazardous?
Moderate to severe irritant to the skin and eyes.
What is eslicarbazepine 400 mg used for?
Eslicarbazepine is utilized either on its own or alongside other medications to manage a specific type of seizure disorder (focal seizures)
What are the side effects of taking eslicarbazepine?
- Agitated
- Irritable, or showing other unusual behaviors, such as experiencing sadness or hopelessness, becoming easily upset, or feeling anxious, restless, or aggressive
What are the blood levels for eslicarbazepine?
Trough plasma levels after administering doses of 400-2400 mg/day ranged from 2 to 28 mcg/mL.
How effective is eslicarbazepine?
24-week retention rates were 81.8 % and 63.8 %
How does eslicarbazepine work?
Eslicarbazepine is believed to function by inhibiting 'voltage-gated sodium channels', preventing sodium from entering the nerve cells. This leads to a decrease in the activity of the nerve cells in the brain, which lowers both the intensity and frequency of seizures.
What should I avoid while taking eslicarbazepine?
Avoid driving, using machinery, or participating in any potentially dangerous activities that require mental alertness and motor coordination.