Eurythmic, Amiodarone
- Introduction to Eurythmic, Amiodarone
- Eurythmic, Amiodarone Composition
- Amiodarone Mechanism of Action
- Eurythmic, Amiodarone Uses
- Off-Label Uses of Amiodarocne
- Eurythmic, Amiodarone Dosage
- Symptoms of Overdosage
- Immediate Actions and Antidote Information
- Amiodarone Dose
- Amiodarone Maintenance Dose
- What Is the Lowest Dose of Amiodarone
- Maximum Dose of Amiodarone in 24 Hours
- Amiodarone Monitoring
- Amiodarone Loading Dose IV
- Recommended Dosage for Different Conditions
- Modifications in Dosage Based on Patient Response
- Eurythmic, Amiodarone Side Effects
- Overview of Common and Serious Side Effects
- Managing Side Effects in Long-term Use
- Incidence and Management Strategies
- Monitoring for Early Detection
- Amiodarone Side Effects in the Elderly
- Amiodarone Side Effects on Blood Pressure
- Amiodarone Blue Skin
- How Long Do Side Effects Last After Stopping Amiodarone?
- Amiodarone Induced Hypothyroidism
- Eurythmic, Amiodarone Warning and Interactions
- Pre-existing Conditions and Amiodarone Usage
- Environmental and Dietary Considerations
- Common and Significant Interactions
- Managing Interaction Risks with Other Medications
- Does Amiodarone Lower Blood Pressure?
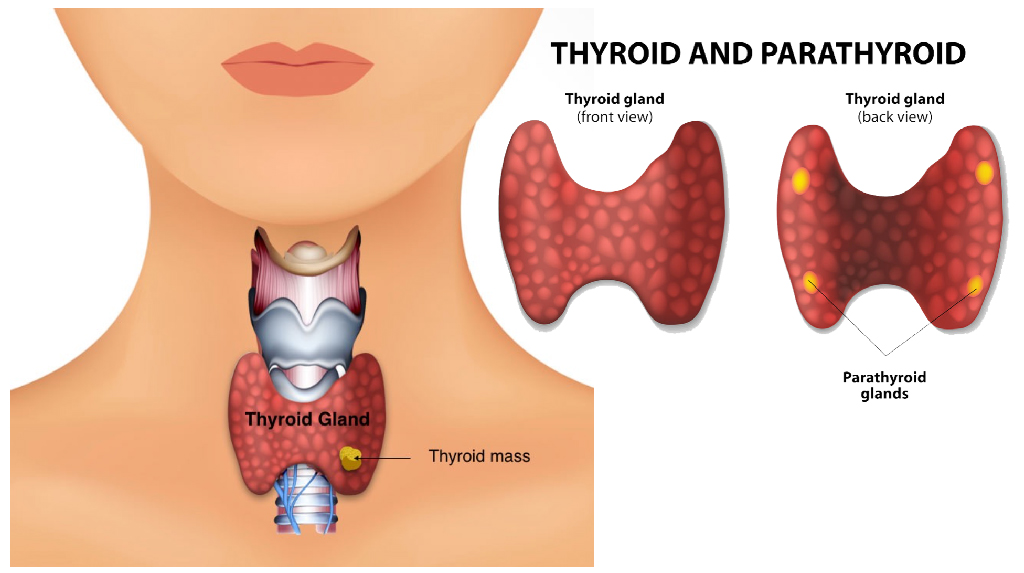
- Amiodarone and Thyroid
- Amiodarone Liver Toxicity
- How Does Amiodarone Cause Liver Damage?
- Does Amiodarone Lower Heart Rate?
- Amiodarone and Alcohol
- Eurythmic, Amiodarone Contradictions and Special Considerations in Administration
- Â
Introduction to Eurythmic, Amiodarone
Amiodarone, sold under the brand name Eurythmic is a widely known medication for treating different types of heart rhythm disorders.
From intervention to ongoing care Amiodarone offers promise to individuals with persistent rhythm issues not responsive, to alternative therapies.
Amiodarone
Overview of Amiodarone
Amiodarone, known for its antiarrhythmic properties is widely effective in managing various types of fast heart rhythms such as ventricular and supraventricular arrhythmias.
Its pharmacological characteristics stand out due to its capability to influence several heart ion channels playing a crucial role in its comprehensive strategy, for managing arrhythmias.
Historical Background and Development
- In the 1960s Belgian pharmacologist Dr. Paul Binet developed Amiodarone initially for angina pectoris treatment.
- The drug's antiarrhythmic effects came to light paving the way for its approval and extensive application in treating arrhythmias by the late 1980s.
- The progression of Amiodarone signifies a change, in medical approaches, where an unexpected finding greatly influenced cardiology treatments.
Significance in Cardiac Treatment
Amiodarone plays a role in treating heart conditions by influencing the electrical properties of the heart muscle. Its lasting effects and significant impact on prolonging the hearts action potential set it apart.
These qualities guarantee effectiveness and strength establishing it as an element in treating serious heart rhythm issues. Additionally its flexibility enables its use in emergency situations. As part of ongoing treatment plans highlighting its unparalleled importance, in cardiac care.
Eurythmic, Amiodarone Composition
Amiodarone marketed as Eurythmic is a medication mainly prescribed for managing severe heart rhythm disorders.
Its formula consists of a combination of active components and additives each playing a role, in its unique medical characteristics.
Active Ingredients
Amiodarone's main active component is amiodarone hydrochloride. It plays a role in regulating heart rhythms by interacting with different ion channels like sodium, potassium, and calcium channels along, with adrenergic receptors.
Excipients and Their Functions
- Lactose is included as a filler to help maintain the stability of the tablet form.
- Magnesium stearate functions, as a lubricant improving the manufacturing process and the drugs absorption.
- Povidone acts as a binder to ensure that the tablet breaks down properly after it is swallowed.
Is Amiodarone a Beta Blocker?
Some people mistakenly believe that Amiodarone is a beta blocker. It actually falls under the category of antiarrhythmic drugs.
While it does have some properties to beta blockers its main function is to extend the repolarization phase of the cardiac action potential.
Adenosine vs Amiodarone
Adenosine works quickly. Is mainly used for treating sudden supraventricular tachycardias whereas Amiodarone has a wider range of effects making it effective, for both ventricular and atrial arrhythmias lasting longer periods.
Dronedarone vs Amiodarone
Dronedarone has a structure similar to Amiodarone but contains less iodine leading to fewer thyroid-related side effects. Nonetheless Amiodarone is still the best choice, for treating severe arrhythmias because of its well established history and effectiveness.
Multaq vs Amiodarone
Multaq, also known as Dronedarone has a profile with fewer side effects on organs when compared to Amiodarone. However, it is generally considered to be less effective. It Is not advised for individuals, with severe heart failure.
Atropine vs Amiodarone
Atropine is commonly employed to address bradycardia serving as a short-term solution while Amiodarone is used to control types of irregular heart rhythms offering a lasting remedy, for maintaining normal heart rhythm.
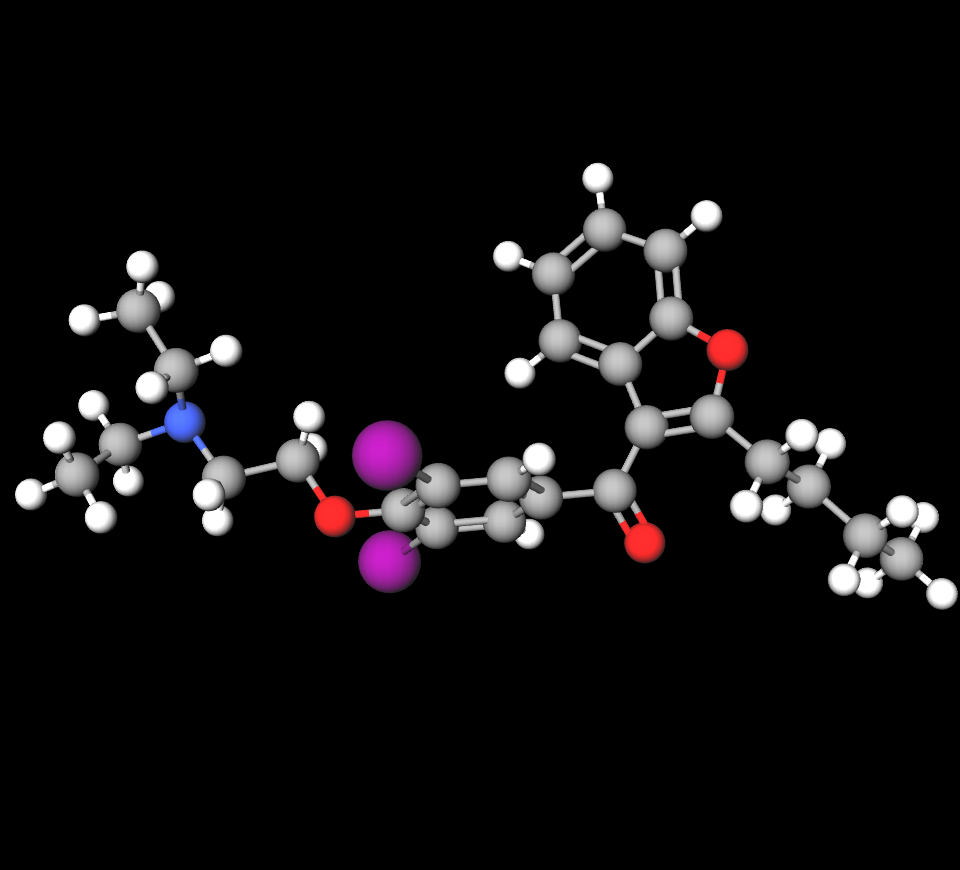
Amiodarone Mechanism of Action
Amiodarone is known for its ranging effects on heart cells mainly used to treat heart rhythm abnormalities. Its diverse influence on cell electrophysiology positions it as a player, in treating atrial and ventricular irregularities.

Mechanism of Action in Cardiac Cells
Amiodarone affects the hearts functions by changing how ions move through cells, which is vital for controlling the hearts electrical activities. Specifically, it blocks sodium and potassium ion channels stabilizes the membranes of cells, and acts as a noncompetitive antagonist to adrenergic receptors.
- By blocking potassium channels Amiodarone extends phase 3 of the cardiac action potential leading to a heart rate.
- Inhibiting sodium channels decreases the excitability of tissues helping to prevent fast and irregular electrical signals.
- Its interaction with calcium channels lowers excitability and conductivity playing a crucial role, in managing arrhythmias originating above the ventricles.
Effects on Heart Rhythm and Conduction
The effectiveness of Amiodarone in therapy is clear as it can effectively alter heart rhythm and conduction pathways. By adjusting the conductivity and refractory period of cardiac tissues it helps restore regular rhythm and improve heart performance. This results in symptom management and a decrease, in the likelihood of arrhythmia reoccurrence.
Amiodarone Half-Life
Amiodarones pharmacokinetics are characterized by a long half-life spanning from 20 to 100 days. This prolonged half-life enables drug concentrations, in the blood enabling continuous regulation of heart rhythm irregularities. However, it requires monitoring to prevent the build-up of harmful effects.
Is Amiodarone a Beta Blocker?
While Amiodarone does have some beta-blocking characteristics like blocking receptors it is mainly categorized as a Class III antiarrhythmic medication. Its beta-blocking impact is seen as an secondary aspect compared to its primary role, in affecting potassium and sodium channels.
Eurythmic, Amiodarone Uses
Amiodarone marketed as Eurythmic is a drug in the field of cardiology mainly used for its ability to treat irregular heart rhythms. It is effective in managing types of heart rhythm disorders providing healthcare providers with a valuable option, for tackling challenging arrhythmias that may not improve with other therapies.
Approved Indications in Cardiology
Amiodarone is formally sanctioned for treating forms of heart rhythm disorders. These encompass;
- Ventricular fibrillation, is a highly unstable state necessitating urgent action.
- Ventricular tachycardia, is defined by an irregular heartbeat.
- Specific varieties of tachycardias when alternative therapies prove ineffective or unsuitable.
Amiodarone in Treating Ventricular and Supraventricular Arrhythmias
The reason why Amiodarone is effective in treating types of heart arrhythmias is because it helps to stabilize the hearts electrical activity. It works by altering the ion flow, in the heart muscle cells, which lowers their excitability and conductivity ultimately restoring a heartbeat and stopping further irregularities from happening again.
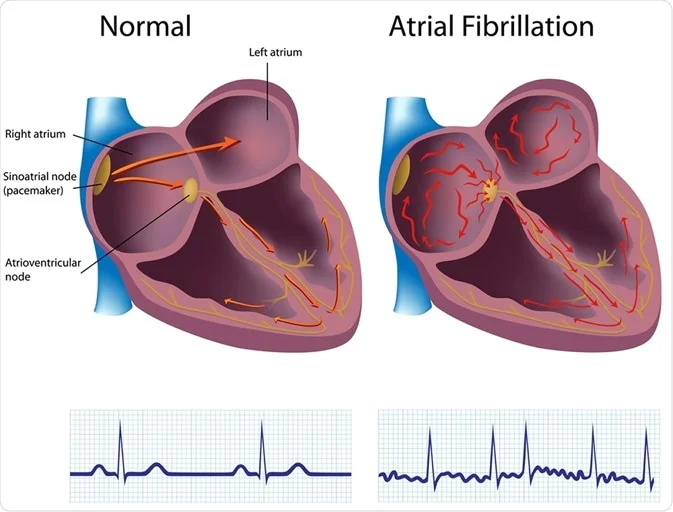
Amiodarone for AFib
Amiodarone works well for treating atrial fibrillation (AFib) a prevalent and intricate heart rhythm disorder. When used for AFib it helps control the heart's rhythm and pace as part of a comprehensive care plan to lower the chances of stroke and enhance overall well-being.
First Dose of Amiodarone in ACLS
This first dose plays a role in quickly restoring the heart's rhythm to improve the likelihood of the patient's survival and neurological outcome.
Amiodarone Treatment for Atrial Fibrillation
Managing fibrillation using Amiodarone requires a delicate equilibrium between dosage and supervision to enhance treatment effectiveness while reducing adverse reactions.
Due to its duration of action and strong impact, on cardiac tissues it is often chosen when alternative antiarrhythmic medications do not offer satisfactory management.
Off-Label Uses of Amiodarocne
Amiodarone a drug commonly used for treating heart rhythm issues in cardiology is often utilized for purposes beyond its intended applications.
These alternative uses to showcase the medication's pharmacological characteristics enabling it to be beneficial, in various clinical situations that were not part of its initial approval.
Common Off-Label Treatments
While Amiodarone is officially approved for the treatment of ventricular arrhythmias and atrial fibrillation healthcare professionals often recommend it for additional purposes;
- Heart Rate Management in Critical Care; Used to control heart rate in critically ill patients when other drugs may not be suitable.
- Preventative Measures After Cardiac Surgery; Given to prevent the development of arrhythmias following heart surgeries, a complication post operation.
- Managing Heart Arrhythmias, in Pediatric Patients; Utilized in scenarios where congenital or acquired arrhythmias pose unique challenges that other medications may not effectively address.
Research and Emerging Off-Label Applications
Recent studies have shed light on potential uses for Amiodarone that could broaden its applications in the medical field;
- Neuroprotective Effects; Research indicates that Amiodarone might offer protection against neurodegenerative processes, which could be beneficial in conditions like Alzheimer's disease.
- Antiviral Properties; There is growing evidence supporting the use of Amiodarone in fighting certain viral infections that lead to inflammation of cardiac tissue.
- Cancer Treatment; Clinical investigations have looked into how effective Amiodarone can be in enhancing the impact of radiation therapy particularly in tumors that are resistant to treatment.
As research advances the role of Amiodarone, in cardiology and other medical areas is evolving, highlighting its versatility and therapeutic potential.
Eurythmic, Amiodarone Dosage
Symptoms of Overdosage
An excessive intake of Amiodarone may result in a range of symptoms. Seeking medical help is vital. These symptoms could involve;
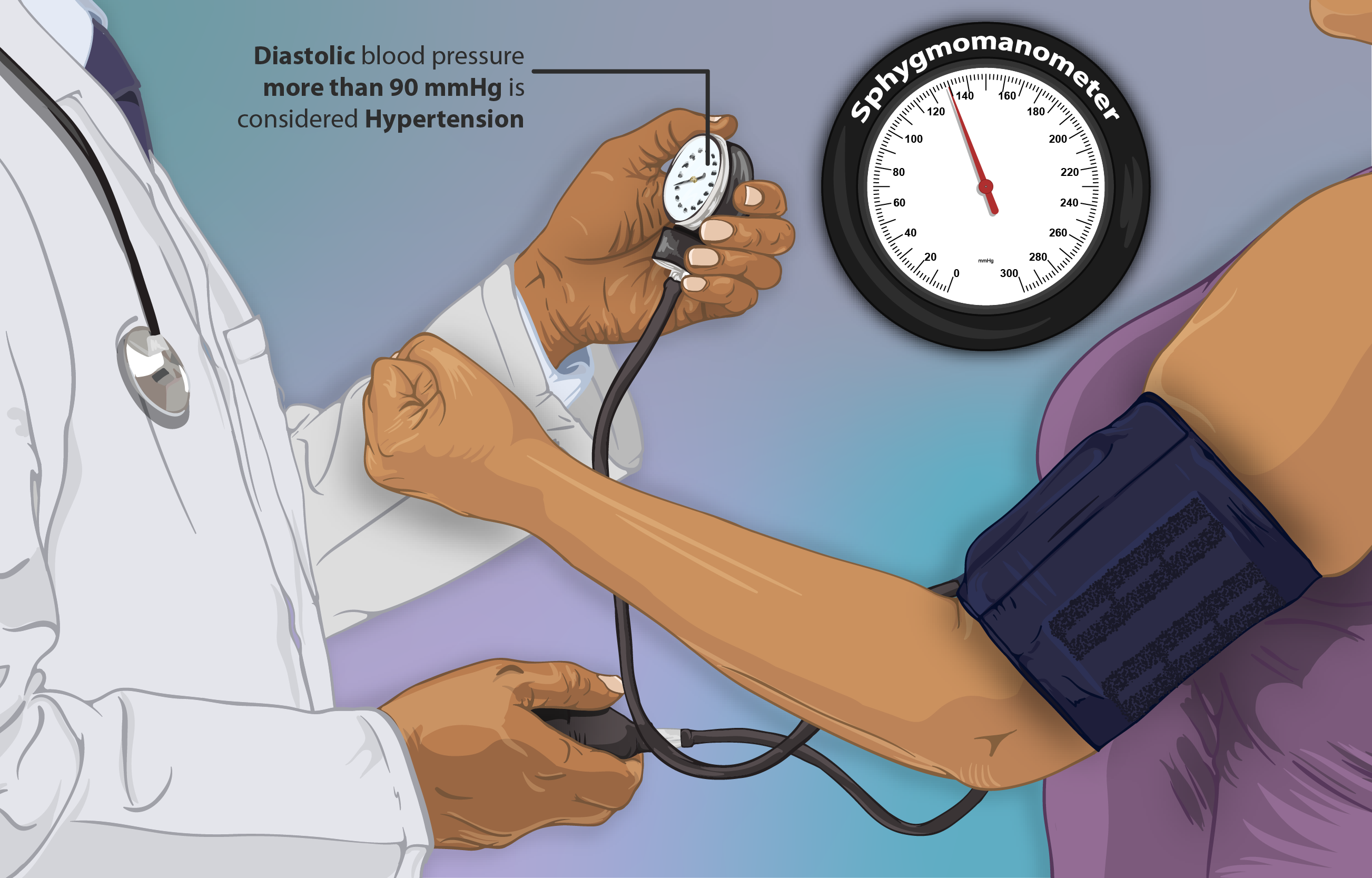
- slowing of the heart rate leading to a cardiac arrest. Pronounced drop in blood pressure.
- Breathing difficulties, which could advance to lung damage.
- Swift identification and intervention play a role, in reducing the harmful impact of an overdose.
Immediate Actions and Antidote Information
In cases of an overdose of Amiodarone, action is necessary; Utilize cardiovascular support methods like atropine for bradycardia. Administer intravenous vasopressors for hypotension.
There is no antidote available; treatment mainly involves supportive and symptomatic care. It is crucial to have care monitoring, in place to effectively address and counteract the overdose effects.
Amiodarone Dose
Then the dosage is gradually decreased to a maintenance level once the desired therapeutic levels are reached. It is crucial to tailor the dosage to each individual to ensure the treatment results while minimizing any potential negative impacts.
Amiodarone Maintenance Dose
Following the phase of loading it is essential to continue with maintenance dosing to uphold the desired therapeutic levels;
- Generally, daily maintenance doses fall within the range of 200 to 400 mg.
- Adjustments to the dosage might be needed depending on how the patient responds and any side effects experienced.
- It is important to monitor drug levels to help determine if adjustments in dosage are necessary.
The aim is to strike a balance, between effectiveness and how well it is tolerated.
What Is the Lowest Dose of Amiodarone
Finding the amount of Amiodarone that works without causing harm is essential;
- Usually, a daily dose of 100 200 mg is considered effective. People who weigh less or are more sensitive might need smaller doses.
- Adjusting the dosage to the least amount that works well can reduce potential long term side effects.
- Specific traits of each patient determine the minimal dose.
Maximum Dose of Amiodarone in 24 Hours
The allowable amount of Amiodarone in a day should not be surpassed to prevent toxicity;
- In urgent situations, a maximum of 1.2 grams per day might be needed during the initial phase.
- For long term use the daily dosage should not go beyond 600 mg.
- Going over these thresholds raises the chances of side effects. It is crucial to follow the advised doses, for patient well-being.
Amiodarone Monitoring
To effectively manage Amiodarone therapy it is important to conduct monitoring, which includes;
- Regular ECGs to identify any arrhythmias and QT prolongation.
- Liver function tests and Thyroid function tests should be done every 6 months.
- If respiratory symptoms arise pulmonary function tests are recommended.
- Regular monitoring plays a role, in detecting potential complications at an early stage.
Amiodarone Loading Dose IV
Administering Amiodarone through loading doses is common in emergency situations to achieve rapid results;
The initial dosage usually consists of 150 mg given intravenously over a period of 10 minutes. This is followed by a maintenance dose of 1 mg per minute for 6 hours then reduced to 0.5 mg per minute for 18 hours.
Once the patient's condition stabilizes the transition to medication is initiated. The use of IV loading helps swiftly reach the required levels, in critical scenarios.
Recommended Dosage for Different Conditions
The recommended amount of Amiodarone may vary based on the specific heart condition being treated.
- For Ventricular Arrhythmias the usual approach involves starting with a dose of 800 to 1600 mg per day for 1 to 3 weeks adjusting as needed until desired results are achieved then transitioning to a daily maintenance dose of 400 mg.
- In cases of Atrial Fibrillation, a dose ranging from 600 to 800 mg per day is typically prescribed for a few weeks before reducing to a maintenance dose, between 200 and 400 mg daily depending on how well the patient responds and any potential side effects.
These dosages are designed to reach therapeutic levels aiding in prompt control of heart rhythm irregularities and stabilizing the patients health status.
Modifications in Dosage Based on Patient Response
Adjustments in the dosage of Amiodarone may be necessary depending on how it works and how well it is tolerated, guided by clinical evaluations and test results.
- It is important to monitor liver and thyroid function as well as check for any pulmonary issues as Amiodarone can have side effects on these organs.
- Changes in dosage may be required based on these assessments. In response to signs of toxicity or inadequate response to treatment, the dosage may need to be increased or decreased accordingly.
- If severe side effects occur, stopping the use of Amiodarone may be necessary. Since individuals metabolize Amiodarone differently some patients may need lower doses to reach therapeutic levels that work best for them.
These adjustments are crucial, in ensuring that Amiodarone delivers its intended benefits while minimizing potential risks and adverse effects.
Eurythmic, Amiodarone Side Effects
Amiodarone, known by the brand name Eurythmic is useful for addressing heart rhythm issues but comes with a wide array of potential side effects. These may vary in intensity requiring observation and control particularly, during extended treatment periods.
Overview of Common and Serious Side Effects
Amiodarone can lead to a variety of side effects.
- Typical ones like nausea, vomiting, fatigue and tremors can usually be controlled by adjusting the dosage or providing relief.
- However severe side effects such, as lung problems, liver issues and thyroid abnormalities need medical care as they could be dangerous.
Managing Side Effects in Long-term Use
Taking Amiodarone for a period requires proactive measures to manage potential side effects.
- It's important to check the functioning of vital organs like the lungs, liver, and thyroid through clinical assessments and lab tests for early identification and intervention.
- Adjusting the dosage of Amiodarone or considering treatment options may be required if side effects become unbearable or pose risks, to health.
Incidence and Management Strategies
The occurrence of side effects differs depending on the dosage how long the medication is taken and the individual's susceptibility. Ways to handle side effects involve educating patients about symptoms scheduling regular follow-up visits and adjusting treatments to suit each patient.
Monitoring for Early Detection
Detecting side effects early can greatly enhance treatment results. It's important to conduct regular tests to monitor how Amiodarone affects the body's organ systems, especially in spotting any signs of toxicity.
Amiodarone Side Effects in the Elderly
Elderly individuals might show heightened sensitivity to Amiodarone, necessitating dosage supervision and vigilant monitoring, for indications of toxicity particularly related to the lungs and heart.
Amiodarone Side Effects on Blood Pressure
Amiodarone could lead to high blood pressure especially when given intravenously in urgent medical situations. Keeping an eye on blood pressure levels and making changes, to the infusion speed can assist in controlling this side effect.
Amiodarone Blue Skin
An uncommon yet significant adverse reaction involves the emergence of a greyish tint, on the skin, particularly in sun-exposed regions referred to as photodermatitis.
How Long Do Side Effects Last After Stopping Amiodarone?
The effects of Amiodarone can last for a period even, after stopping the medication varying based on how long it was taken and the patient's metabolism.
Amiodarone Induced Hypothyroidism
Amiodarone has the potential to impact thyroid function, which may result in hypothyroidism. Treatment involves conducting thyroid function assessments and administering thyroid hormone replacement therapy if needed.
Eurythmic, Amiodarone Warning and Interactions
Eurythmic, also known as Amiodarone is a medication used to treat heart rhythm problems. It comes with caution and can interact with other drugs so it's crucial to take these factors into account to prevent any negative outcomes and ensure the best possible treatment results.
Pre-existing Conditions and Amiodarone Usage
Patients with existing health issues should be careful when taking Amiodarone.
- Those with thyroid problems should be cautious because Amiodarone could affect their thyroid function possibly causing either an overactive thyroid.
- People with lung conditions need to be mindful of the risk of pulmonary toxicity from long-term use of Amiodarone.
- Additionally, individuals, with liver disease should undergo monitoring since Amiodarone might worsen their liver function.
Environmental and Dietary Considerations
Environmental elements and dietary choices may impact how well Amiodarone works and the potential side effects it may cause. It's advisable to limit sun exposure to reduce the risk of developing photodermatitis linked to Amiodarone. Additionally, it is recommended to steer off grapefruit juice and foods rich, in iodine as they can modify how Amiodarone is absorbed by the body and disrupt its metabolism.
Common and Significant Interactions
Amiodarone can have interactions with medications, which could result in significant health concerns. When taken together with anticoagulants such, as warfarin there is a risk of bleeding. Additionally combining it with statins may elevate the chances of experiencing statin-induced myopathy and rhabdomyolysis.
Managing Interaction Risks with Other Medications
Managing interactions with the drug Amiodarone involves keeping an eye on both the levels of the drug and any symptoms experienced by the patient when they are taking other medications that could potentially interact with Amiodarone. It's important to adjust dosages or switch to medications, with safer interaction profiles as needed.
Does Amiodarone Lower Blood Pressure?
Amiodarone and Thyroid
The effects of Amiodarone, on the thyroid gland are intricate requiring frequent thyroid function tests to identify any issues and address them effectively.
Amiodarone Liver Toxicity
Amiodarone can lead to liver problems showing as liver enzyme levels and possible serious liver damage.
How Does Amiodarone Cause Liver Damage?
The liver damage caused by Amiodarone is believed to occur when the harmful byproducts of the medication build up in the liver leading to stress and harm, to the cells gradually.
Does Amiodarone Lower Heart Rate?
Amiodarone has the ability to reduce heart rate by impacting the heart's conduction system especially when used to treat fast heart rhythms.
Amiodarone and Alcohol
Avoid consuming alcohol when taking Amiodarone to reduce the chance of liver damage as it can worsen the medications impact, on the liver potentially leading to risks of hepatotoxicity.
Eurythmic, Amiodarone Contradictions and Special Considerations in Administration
Amiodarone in Elderly Patients
Amiodarone, a medication for heart rhythm issues needs to be given with great care to older patients. The changes that come with aging like kidneys working effectively how the body responds to drugs changing and having more health problems mean that the dosage needs to be adjusted and monitoring needs to be done carefully.
Because the body clears out the drug slower in people lower doses are needed. Older patients are more likely to have reactions like slow heart rate and low blood pressure. It's really important to do regular heart monitoring tests to catch any harmful effects on heart rhythm. Adjusting doses carefully and checking regularly are crucial, for making sure the treatment works well without causing many risks.
Use in Pregnant Women and Nursing Mothers
Breastfeeding mothers may pass on the drug to their babies through breast milk. It is advisable to opt for antiarrhythmic treatments unless the benefits to the mother outweigh the risks to the fetus. It is crucial to obtain consent and engage in detailed discussions, with patients regarding potential dangers.
Pediatric Use: Safety and Efficacy
Using Amiodarone in children requires an approach as there are not many studies on its safety and effectiveness. It is important to consider the risks and benefits before prescribing it. Adjusting the dosage according to the child's body surface area is essential.
Children are at risk of thyroid problems when taking this medication. Regular monitoring, for liver and lung issues is necessary. Pediatric heart specialists need to be cautious and follow guidelines to give the medication safely.
Amiodarone Contraindications
There are reasons why Amiodarone should be used cautiously requiring careful consideration when selecting patients. Absolute contraindications involve; reactions to the medication. Significant issues with sinus node function or atrioventricular block. Fainting is caused by slow heart rate. Relative contraindications call for an evaluation of risks particularly in individuals, with existing thyroid or lung problems.
Amiodarone Toxicity
Amiodarone toxicity poses a risk often leading to the need to stop treatment. It can affect parts of the body such, as;
- Lung issues; scarring, and inflammation.
- Liver problems; increased liver enzyme levels, hepatitis.
- Thyroid irregularities; underactive thyroid. It's important to recognize and address these issues to prevent lasting harm.
Amiodarone Toxicity Symptoms
It is essential to identify signs of Amiodarone toxicity on for swift intervention. Symptoms to watch out for include;
- Shortness of breath and coughing which may indicate lung issues. Yellowing of the skin and abdominal discomfort hinting at liver problems.
- Feeling tired changes in weight or fluctuations, in weight that could signal thyroid irregularities.
- Healthcare professionals need to stay vigilant and carry out tests promptly to diagnose the condition accurately.
Handling and Storage of Amiodarone
Recommended Storage Conditions
Storing Amiodarone correctly is crucial to keep it effective and stable. It's best to; Keep it at a controlled room temperature, between 15 30°C (59 86°F). Shield it from light and moisture.
Always make sure the container is tightly sealed when you're not using it. Adhering to these instructions helps maintain the medications potency.
Stability and Shelf Life
Amiodarone has a lasting shelf life when stored correctly. Important factors to keep in mind are;
- Following the expiration dates given by the manufacturer.
- Keeping it away from extreme temperatures.
- Periodically inspecting for any alterations in its appearance like color changes or forming crystals.
By adhering to these guidelines you can guarantee that the medication stays potent, for the duration of its shelf life.
Stopping Amiodarone
Stopping the use of Amiodarone should be done with caution and preparation in mind;
- It may be necessary to reduce the dosage to avoid sudden arrhythmias.
- Keeping an eye out for any lingering effects due to the drugs half life.
- Switching, to an antiarrhythmic medication if required.
- Taking a strategic approach when discontinuing Amiodarone helps mitigate potential risks linked to its withdrawal.