1. Introduction
Galamer, containing the active compound Galantamine hydrobromide, is a therapeutic agent classified under cholinesterase inhibitors. It plays a crucial role in the management of neurodegenerative conditions characterized by cognitive decline and memory deterioration. Initially derived from the bulbs of the snowdrop plant (*Galanthus nivalis*), Galantamine’s development marked a significant advancement in neuropharmacology due to its dual modulatory activity on cholinergic neurotransmission.
Its primary clinical application lies in the treatment of Alzheimer’s disease and related dementias, where it enhances neuronal communication and delays cognitive impairment progression. Galamer remains a cornerstone in symptomatic therapy, offering measurable improvements in memory, attention, and functional ability.
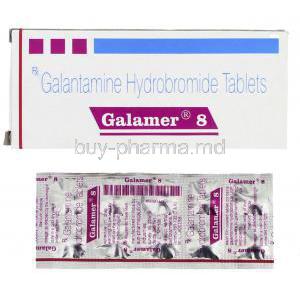
2. Composition and Formulation
The principal active ingredient in Galamer is Galantamine hydrobromide, a tertiary alkaloid known for its reversible inhibition of acetylcholinesterase.
It is available in multiple pharmaceutical forms tailored for patient-specific needs, including:
- Immediate-release tablets
- Extended-release capsules
- Oral solution for flexible dosing
Strength variations typically include 4 mg, 8 mg, 12 mg, 16 mg, and 24 mg formulations, allowing gradual titration and long-term maintenance. Inactive components may include lactose monohydrate, magnesium stearate, microcrystalline cellulose, and hypromellose, depending on formulation type.
Globally, Galantamine is marketed under various trade names such as Razadyne, Reminyl, and Galamer, produced by reputable pharmaceutical companies ensuring consistent efficacy and safety.
3. Mechanism of Action – How Galamer Works
The therapeutic essence of Galamer lies in its ability to potentiate acetylcholine-mediated neurotransmission within the central nervous system. Acetylcholine is vital for learning, memory consolidation, and neuronal signaling — all of which deteriorate in Alzheimer’s pathology.
Galantamine exerts a dual mechanism of action:
- Reversible inhibition of acetylcholinesterase: Prevents enzymatic breakdown of acetylcholine, thereby increasing synaptic concentration and enhancing cognitive signaling.
- Allosteric modulation of nicotinic acetylcholine receptors: Enhances receptor sensitivity and stimulates additional acetylcholine release, supporting neuroplasticity and synaptic repair.
This unique bimodal mechanism distinguishes Galamer from other cholinesterase inhibitors such as Donepezil and Rivastigmine, conferring a broader therapeutic spectrum and potential neuroprotective effects.
4. Therapeutic Uses
4.1 Approved Uses
Galamer is clinically indicated for:
- Mild to moderate Alzheimer’s disease – improves cognitive and behavioral symptoms.
- Vascular dementia – supports cognitive processing in patients with cerebrovascular impairment.
- Cognitive dysfunction in Parkinson’s disease – enhances attention and executive function.
4.2 Off-label Uses
Emerging evidence supports Galamer’s potential beyond Alzheimer’s therapy, including:
- Mild cognitive impairment (MCI) and age-related memory decline
- Post-stroke cognitive dysfunction rehabilitation
- Traumatic brain injury recovery – improvement of neural connectivity
- Schizophrenia-associated cognitive deficits
- Autism spectrum disorder cognitive modulation (experimental)
5. Dosage and Administration
Treatment initiation typically begins with 4 mg twice daily, gradually titrated at 4-week intervals to minimize gastrointestinal intolerance. The maintenance dose generally ranges from 16 mg to 24 mg per day, depending on individual tolerance and therapeutic response.
To enhance absorption and reduce nausea, the medication should be administered with food and accompanied by adequate hydration.
If a dose is missed, it should be skipped if the next scheduled dose is near—double dosing is discouraged. Patients discontinuing treatment for several days should resume from the lowest tolerated dose. Extended-release capsules are taken once daily, preferably in the morning, while immediate-release tablets are dosed twice daily.
6. Side Effects
6.1 Common Side Effects
Typical adverse reactions may include:
- Nausea, vomiting, and diarrhea
- Dizziness or lightheadedness
- Headache and fatigue
- Loss of appetite and mild weight reduction
- Insomnia or vivid dreams
6.2 Serious Adverse Effects
In rare instances, Galamer may cause:
- Bradycardia and fainting episodes
- Gastrointestinal bleeding, particularly in patients with ulcer history
- Seizures or exacerbation of existing epilepsy
- Urinary retention or dehydration
- Hypersensitivity reactions such as rash or dermatitis
7. Drug Interactions
Galamer may interact with multiple pharmacological agents, necessitating careful supervision:
- Anticholinergic drugs (e.g., atropine) – reduced therapeutic efficacy.
- Other cholinesterase inhibitors – additive toxicity.
- CYP2D6 and CYP3A4 inhibitors (e.g., ketoconazole, paroxetine) – elevated plasma concentration of Galantamine.
- Beta-blockers and calcium channel blockers – increased risk of bradycardia.
- Alcohol and CNS depressants – enhanced sedation or confusion.
- Potential interaction with antidepressants and antipsychotics affecting CNS signaling.
8. Warnings and Important Precautions
Caution is warranted in individuals with cardiovascular, gastrointestinal, or metabolic vulnerabilities.
Key precautions include:
- Monitor for cardiac conduction abnormalities, particularly in patients with sick sinus syndrome.
- Increased risk of peptic ulcer or gastrointestinal bleeding.
- Monitor elderly patients for syncope, dizziness, and falls.
- Adjust dosage in renal or hepatic impairment to prevent accumulation.
- Gradual dose escalation is vital to avoid cholinergic overload.
- Discontinue Galamer prior to surgical anesthesia to prevent exaggerated vagal response.
9. Contraindications
Galamer is contraindicated in patients with:
- Known hypersensitivity to Galantamine or formulation excipients
- Severe hepatic or renal impairment
- Concurrent administration of other cholinesterase inhibitors
- Uncontrolled cardiac arrhythmia or sick sinus syndrome
- Active peptic ulcer disease with bleeding or perforation
The medication should be prescribed only under medical supervision, with continuous evaluation of benefits versus potential risks in each patient.
10. Careful Administration
Administration of Galamer requires vigilant medical supervision, particularly in individuals with coexisting health conditions. The drug’s cholinergic action may amplify or complicate underlying disorders, necessitating tailored management strategies.
Patients with asthma, chronic obstructive pulmonary disease (COPD), or other pulmonary disorders should be monitored for bronchospasm or respiratory distress. Cholinergic stimulation may increase bronchial secretions and airway reactivity, especially in predisposed individuals.
For patients with epilepsy or seizure history, Galamer should be administered cautiously, as it may lower the seizure threshold due to enhanced cholinergic activity in the central nervous system. Regular neurological evaluation is advisable to detect early manifestations of convulsions.
Maintenance of adequate hydration and monitoring of body weight are crucial, as nausea and vomiting may lead to dehydration and metabolic imbalance during dose escalation. Patients with urinary outflow obstruction, such as those with benign prostatic hypertrophy, require close surveillance, as Galamer may increase detrusor muscle tone and aggravate urinary retention.
A gradual and carefully supervised dose escalation phase minimizes adverse effects while enhancing tolerability. Rapid titration or noncompliance during adjustment may result in cholinergic overactivity and cardiovascular complications.
11. Administration in Special Populations
11.1 Administration to Elderly
Elderly patients represent the primary demographic for Galamer therapy, yet they exhibit increased pharmacokinetic variability and physiological sensitivity. Age-related hepatic and renal decline can alter drug metabolism and excretion, demanding a more cautious approach.
The elderly population is particularly susceptible to cholinergic adverse effects such as dizziness, bradycardia, or gastrointestinal distress. Therefore, treatment should begin with a lower initial dose followed by slow and deliberate titration.
Frequent monitoring for orthostatic hypotension and syncope is essential, as falls in this age group may lead to severe injury. Caregivers should be educated to identify subtle behavioral or physical changes suggestive of intolerance.
11.2 Administration to Pregnant Women and Nursing Mothers
Galamer is classified as Pregnancy Category C. Animal studies have demonstrated potential risks to fetal development, yet controlled human studies are insufficient to confirm safety. Consequently, the medication should be prescribed during pregnancy only when the anticipated benefit clearly outweighs potential harm.
Data regarding the excretion of Galantamine into breast milk are limited. However, due to the drug’s lipophilic properties, it is presumed to be present in trace quantities. Breastfeeding women should avoid therapy or suspend nursing if treatment is unavoidable.
Close consultation with a healthcare provider is essential for risk-benefit evaluation in both pregnant and lactating patients, ensuring maternal safety while minimizing fetal or neonatal exposure.
11.3 Administration to Children
The safety and efficacy of Galamer in children under 18 years of age have not been established. Pediatric trials remain limited, and existing studies exploring off-label applications—such as in autism spectrum disorder (ASD) or attention-deficit hyperactivity disorder (ADHD)—are preliminary and inconclusive.
Until more robust evidence becomes available, Galamer is not recommended for pediatric use without strict medical supervision. Any consideration for off-label administration must include continuous clinical observation and parental counseling regarding potential risks.
12. Overdosage
An overdose of Galamer can precipitate a cholinergic crisis characterized by excessive stimulation of the parasympathetic nervous system.
Common manifestations include:
- Severe nausea and vomiting
- Profound bradycardia
- Hypotension and syncope
- Seizures and respiratory depression
Immediate intervention involves gastric lavage to remove unabsorbed drug and aggressive supportive care to stabilize hemodynamic parameters. Administration of atropine sulfate serves as the specific antidote, effectively reversing muscarinic overactivation.
Continuous monitoring of vital signs and cardiac rhythm is critical until clinical stability is achieved. In severe cases, hospitalization and intravenous fluid replacement may be required.
13. Storage and Handling Precautions
Galamer should be stored under controlled conditions to preserve potency and prevent degradation.
Recommended guidelines include:
- Storage temperature: below 30°C in a dry environment
- Protection from direct sunlight and humidity
- Keep out of reach of children and pets
- Do not use beyond the printed expiry date
- Dispose of unused or expired medication responsibly, in accordance with local pharmaceutical waste regulations
Healthcare professionals should follow appropriate handling procedures to prevent cross-contamination or accidental ingestion during dispensing.
14. Patient Counseling and Safety Information
Effective patient education enhances both adherence and therapeutic outcomes. Patients and caregivers should receive clear instructions regarding dosage adjustments and potential side effects.
Key counseling points include:
- Adhere strictly to the prescribed dosage schedule and titration plan
- Report early symptoms such as persistent nausea, dizziness, or fainting
- Maintain adequate hydration and balanced nutrition to counteract gastrointestinal effects
- Attend regular medical follow-up visits for cognitive and cardiovascular assessment
- Immediately inform healthcare providers of unusual mood or behavioral changes
Ongoing monitoring and communication between patient, caregiver, and clinician ensure a safe and effective therapeutic experience.
15. Summary
Galamer remains a pivotal therapy for Alzheimer’s disease and related cognitive disorders, acting through cholinergic enhancement and synaptic modulation. Its clinical success depends on personalized dosing, continuous monitoring, and prudent administration in vulnerable populations.
Ensuring patient compliance and early recognition of adverse effects significantly optimizes treatment efficacy. As research advances, new formulations and broader indications of Galantamine continue to shape the evolving landscape of neurocognitive medicine.