Introduction to OD Phyllin
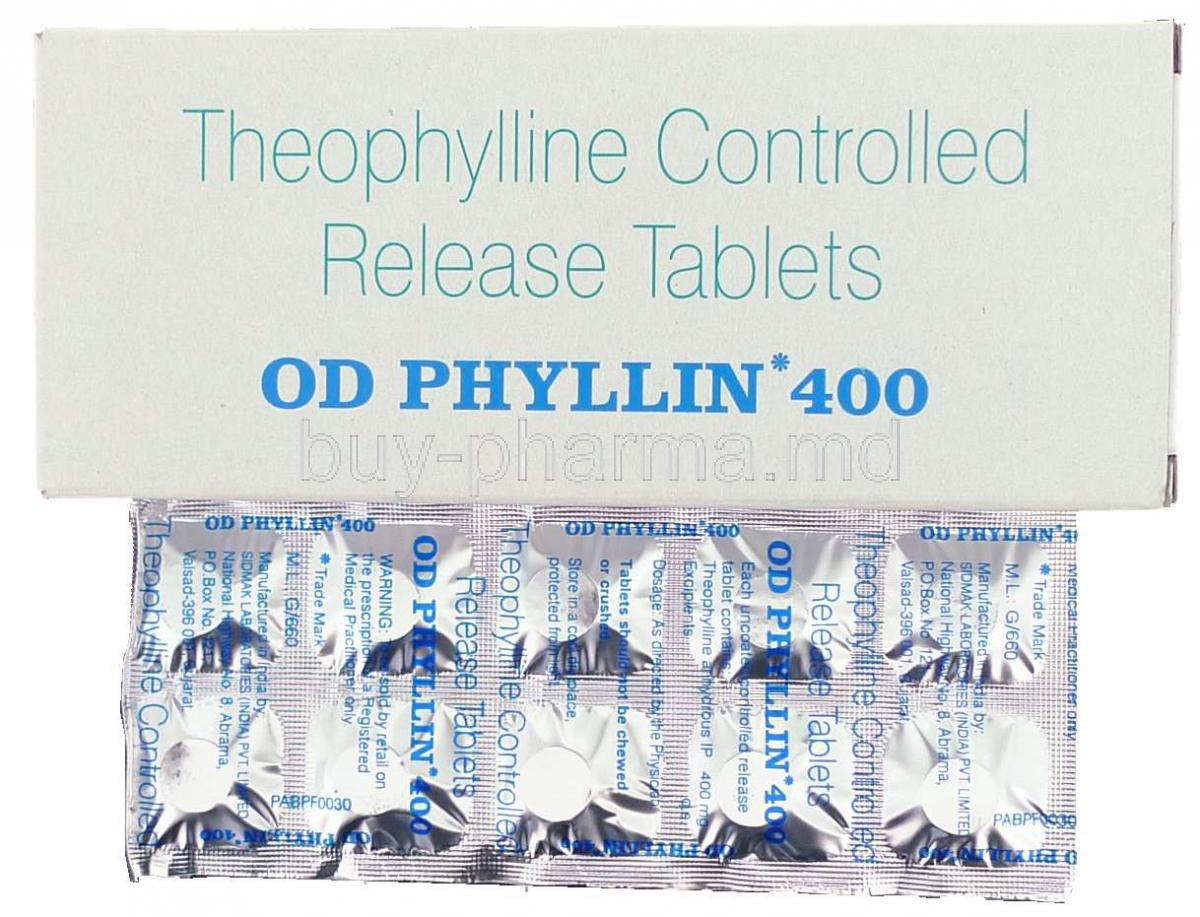
Overview of OD Phyllin as a theophylline preparation
OD Phyllin is an extended-release formulation of theophylline, a methylxanthine bronchodilator designed for once-daily administration. It aims to stabilize airway caliber, reduce nocturnal symptoms, and smooth out peak–trough variability in serum concentrations.
- Once-daily kinetics help improve adherence where multiple daily dosing is impractical.
- Intended for maintenance therapy, not for immediate relief of acute bronchospasm.
Historical background and medical relevance
Theophylline has been used for decades in obstructive airway disease. Its clinical role has narrowed with the rise of inhaled corticosteroids (ICS), long-acting β2-agonists (LABA), and long-acting muscarinic antagonists (LAMA), yet it remains a viable option in selected patients.
- Legacy agent with well-characterized pharmacology and monitoring parameters.
- Particularly considered when cost, access, or inhaler technique issues hinder inhaled regimens.
Therapeutic classification and place in treatment guidelines
Classified as a bronchodilator (methylxanthine). Contemporary guidelines generally position theophylline as adjunctive or alternative maintenance therapy.
- Asthma: add-on in persistent symptoms when optimized inhaled therapy is insufficient.
- COPD: optional adjunct for symptom relief in select patients after first-line therapies.
Composition and Formulation
Active ingredient: Theophylline
Each OD Phyllin tablet contains theophylline in a controlled-release matrix engineered to deliver sustained plasma levels over ~24 hours.
Available strengths and dosage forms
Extended-release tablets in multiple strengths to facilitate weight-based and titration dosing. Availability may vary by market.
- Typical strengths enable incremental up-titration without exceeding therapeutic ranges.
- Scored tablets may permit dose flexibility when permitted by local labeling.
Excipients and inactive ingredients
Formulation commonly includes release-modifying polymers, binders, and stabilizers. Patients with known excipient sensitivities should review product labeling.
Mechanism of Action: How OD Phyllin Works
Pharmacodynamics: phosphodiesterase inhibition and bronchodilation
Theophylline non-selectively inhibits phosphodiesterases (PDE), increasing intracellular cyclic AMP. Elevated cAMP relaxes bronchial smooth muscle and attenuates mediator release.
- Adenosine receptor antagonism contributes to airway smooth-muscle relaxation and reduced bronchoconstrictive signaling.
- Mild diuretic and chronotropic effects may appear at higher exposures.
Impact on smooth muscle relaxation in airways
Bronchial smooth-muscle tone decreases, improving airflow and reducing air-trapping. Patients often report easier nocturnal breathing and less exertional dyspnea once steady-state is achieved.
Anti-inflammatory and immunomodulatory effects
At therapeutic levels, theophylline exhibits modest anti-inflammatory activity, including effects on histone deacetylase-2 (HDAC2) signaling pathways, which may enhance corticosteroid responsiveness in certain phenotypes.
Effect on respiratory drive and diaphragmatic function
Theophylline can stimulate central respiratory centers and augment diaphragmatic contractility, which may support ventilation in specific clinical contexts.
Approved Medical Uses
Asthma management (acute and chronic control)
Indicated for maintenance treatment in asthma to decrease symptom burden and nocturnal awakenings. Not a rescue medication.
- Use as an adjunct to ICS ± LABA when control remains suboptimal.
- Therapeutic drug monitoring (TDM) is integral to safe, effective use.
Chronic obstructive pulmonary disease (COPD) treatment
May reduce dyspnea and improve exercise tolerance in select COPD patients when added to core inhaled therapy.
- Consider in settings where inhaled options are inaccessible or poorly tolerated.
- Monitor closely for cardiovascular effects in multimorbid COPD.
Bronchospasm prevention in chronic lung disorders
Helps blunt bronchospastic episodes in chronic bronchitic and asthmatic phenotypes, particularly with nocturnal symptomatology.
Off-Label Uses
Apnea of prematurity in neonates
Theophylline has been used to stimulate respiratory drive; however, caffeine citrate is generally preferred due to a wider therapeutic window and simpler dosing.
Cheyne–Stokes respiration and sleep apnea syndromes
Historical and niche use to modulate respiratory pattern instability. Evidence is limited; individualized risk–benefit assessment is essential.
Adjunct therapy in pulmonary hypertension
Occasional adjunctive use has been explored to improve ventilatory efficiency. Data remain inconclusive and patient selection is critical.
Potential use in heart failure patients with respiratory compromise
By enhancing diaphragmatic performance and ventilatory drive, theophylline has been investigated in specific heart-failure cohorts; careful monitoring is mandatory due to arrhythmic risk.
Other investigational therapeutic roles
Research continues into anti-inflammatory and steroid-sensitizing properties in refractory airway disease phenotypes.
Dosage and Administration Guidelines
Standard adult dosage recommendations
Dosing is individualized. Initiate conservatively and titrate using TDM to a typical serum trough range of ~5–15 mcg/mL.
- Common starting point (extended-release): 200–300 mg once daily, then adjust every 3–5 days based on levels, response, and tolerability.
- Do not exceed customary maxima without specialist oversight.
Pediatric dosage schedules
Weight-based dosing with strict level monitoring.
- Children often require higher mg/kg than adults due to faster clearance; titrate carefully to target serum range.
- Neonates and infants: markedly variable clearance—specialist protocols and close TDM are requisite.
Extended-release vs. immediate-release formulations
Extended-release (OD) offers smoother pharmacokinetics and improved adherence; immediate-release may be used when finer dose adjustments or split dosing are needed.
- Swallow ER tablets whole; do not crush or chew.
- Maintain consistent timing and relation to meals to reduce variability.
Dosage adjustments in renal or hepatic impairment
Theophylline is hepatically metabolized (notably via CYP1A2; minor CYP3A pathways). Hepatic dysfunction necessitates lower doses and slower titration.
- Renal impairment has less impact on clearance but monitor for metabolite accumulation in severe disease.
- Intercurrent fever, viral illness, or heart failure can reduce clearance—reassess levels during illness.
Monitoring of serum theophylline levels
Therapeutic drug monitoring is central.
- Obtain trough level at steady-state (after ~3 days of unchanged dosing).
- Re-check after dose changes, when adding/removing interacting drugs, and during acute illness.
Instructions for missed doses and overdose management
Missed dose guidance is simple yet crucial.
- If a dose is missed and it is not close to the next scheduled dose, take it when remembered.
- If near the next dose, skip the missed dose. Do not double up.
Overdose can be serious due to a narrow therapeutic index.
- Early symptoms: nausea, vomiting, tremor, agitation, insomnia, tachycardia.
- Severe toxicity: hypokalemia, refractory vomiting, atrial or ventricular arrhythmias, seizures.
- Initial management: activated charcoal (including multiple doses when appropriate), electrolyte correction, benzodiazepines for seizures, cautious β-blockade for tachyarrhythmias where clinically suitable, continuous cardiac monitoring. Escalate per toxicology guidance.
Administration in Special Populations
Elderly Patients: dose adjustment, monitoring for toxicity
Reduced clearance and polypharmacy increase risk. Start low, titrate slowly, and monitor levels meticulously.
- Higher susceptibility to arrhythmias and CNS effects.
- Review interacting drugs routinely (e.g., macrolides, fluoroquinolones, anticonvulsants, smoking status).
Pregnant Women and Nursing Mothers: safety data, placental transfer, breast milk excretion
Theophylline crosses the placenta and is excreted into breast milk.
- Use only if expected benefit justifies potential risk; aim for the lowest effective dose with TDM.
- Monitor mother and infant for irritability, tachycardia, or feeding difficulties if used during lactation.
Children: pediatric safety profile, indications in neonates and infants
Safe use hinges on careful weight-based dosing and frequent monitoring.
- In apnea of prematurity, caffeine is generally preferred; theophylline requires specialist oversight.
- Educate caregivers on dosing precision, symptom recognition, and the importance of scheduled level checks.
This information supports professional counseling. Individualize therapy, adhere to local labeling, and consult a clinician or pharmacist for patient-specific decisions.
Side Effects of OD Phyllin
Common Side Effects
OD Phyllin, containing theophylline, is associated with a range of adverse reactions. Many are mild and transient but still require patient awareness and clinical vigilance.
- Nausea, vomiting, and gastrointestinal discomfort: Early signs of intolerance, often dose-related, and sometimes mitigated by taking the drug with food.
- Headache, dizziness, and insomnia: Central nervous system stimulation may manifest as difficulty sleeping, nervous irritability, or intermittent headaches.
- Palpitations and mild tachycardia: Subtle increases in heart rate may occur, especially in sensitive individuals or at higher serum levels.
Serious Adverse Effects
At elevated concentrations, OD Phyllin may precipitate severe and potentially life-threatening events.
- Seizures and arrhythmias: Neurological and cardiac complications are hallmark features of toxicity.
- Severe hypotension or hypertension: Hemodynamic instability may develop depending on the patient’s baseline cardiovascular status.
- Hypokalemia and metabolic disturbances: Electrolyte derangements can worsen arrhythmic risk and require urgent correction.
Drug Interactions
Interaction with antibiotics (erythromycin, ciprofloxacin)
Certain antimicrobials inhibit hepatic metabolism, markedly raising serum theophylline levels. Clinical manifestations may escalate rapidly.
Effects of smoking, alcohol, and caffeine on metabolism
- Smoking: Induces clearance, potentially lowering drug effectiveness.
- Alcohol: Variable impact on metabolism; chronic intake may enhance clearance, while acute intoxication impairs it.
- Caffeine: Synergistic stimulant effects on the central nervous and cardiovascular systems.
Interaction with anticonvulsants and other bronchodilators
Drugs such as phenytoin or carbamazepine accelerate clearance, reducing efficacy. Co-administration with β2-agonists may amplify cardiovascular stimulation.
Impact of CYP450 inhibitors and inducers on theophylline levels
Theophylline metabolism is highly dependent on CYP1A2 and related isoenzymes. Inhibitors (e.g., fluvoxamine) elevate levels, while inducers (e.g., rifampicin) decrease them, necessitating careful adjustment.
Warnings and Contraindications
Known hypersensitivity to theophylline
Absolute contraindication due to risk of anaphylaxis or severe hypersensitivity reactions.
History of seizure disorders
Lower seizure threshold increases vulnerability; alternative therapies should be prioritized.
Severe cardiac arrhythmias and unstable cardiovascular disease
The chronotropic and inotropic actions of theophylline can exacerbate underlying cardiac instability.
Peptic ulcer disease and gastrointestinal bleeding risks
Theophylline increases gastric acid secretion and may worsen ulcerative conditions.
Relative contraindications in thyroid dysfunction and liver impairment
Both hyperthyroidism and hepatic impairment alter drug metabolism, increasing the likelihood of toxicity.
Careful Administration and Important Precautions
Importance of therapeutic drug monitoring
Theophylline has a narrow therapeutic index, making routine serum level measurement essential for safety and efficacy.
Recognition and early management of toxicity symptoms
- Gastrointestinal upset
- Tremor and agitation
- Unexplained tachycardia or arrhythmia
Early recognition allows timely dose adjustment before complications escalate.
Adjustments in concurrent febrile illness or infection
Infections and fever reduce drug clearance, leading to accumulation. Temporary dose reduction may be warranted.
Caution in patients with multiple comorbidities
Polypharmacy, impaired organ function, and systemic illnesses complicate dosing and necessitate heightened vigilance.
Overdose and Toxicity
Clinical presentation of acute theophylline overdose
Symptoms include relentless vomiting, severe tremors, agitation, tachyarrhythmias, seizures, and profound electrolyte disturbances.
Emergency management: activated charcoal, seizure control, arrhythmia monitoring
- Multiple-dose activated charcoal is a cornerstone of management.
- Benzodiazepines are often required for seizure control.
- Continuous cardiac monitoring ensures timely detection of arrhythmias.
Long-term complications of chronic overdose
Prolonged exposure may lead to persistent neuropsychiatric symptoms, recurrent arrhythmias, and metabolic imbalances requiring extended care.
Handling and Storage Precautions
Recommended storage conditions (temperature, humidity, light)
Keep tablets at controlled room temperature, shielded from direct light, heat, and excessive humidity to maintain potency.
Safe handling instructions for healthcare providers
Healthcare staff should avoid crushing extended-release tablets. Proper labeling and patient education are essential to prevent dosing errors.
Disposal of expired or unused medication
Expired or unused OD Phyllin should be discarded responsibly, following local pharmaceutical waste guidelines to prevent accidental ingestion or environmental contamination.