Introduction to Temonat (Temozolomide)
Overview of Temonat and its Pharmaceutical Classification
Temonat, containing the active compound Temozolomide, belongs to the class of alkylating agents used in oncology. It is categorized as an oral cytotoxic chemotherapeutic drug that exerts profound anti-tumor activity. As a prodrug, it becomes active after spontaneous conversion in physiological conditions, making it unique among oral chemotherapeutics.
Importance of Temozolomide in Cancer Treatment
Temozolomide revolutionized the therapeutic approach to certain aggressive brain tumors. It provides clinicians with a treatment option that penetrates the blood-brain barrier efficiently. Its inclusion in first-line therapy for glioblastoma multiforme has significantly improved survival rates, making it a mainstay in neuro-oncology.
Brand Names and Generic Availability
While Temonat is a widely recognized brand, Temozolomide is also marketed under names such as Temodar and other generics. The availability of generics has expanded patient access globally, reducing treatment costs without compromising efficacy.
Composition and Formulation
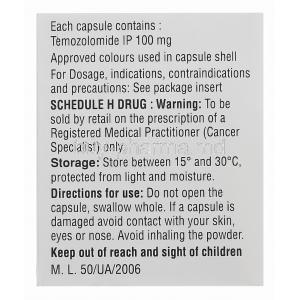
Active Ingredient: Temozolomide
The primary component is Temozolomide, a triazene derivative with potent alkylating activity. Its chemical configuration allows rapid oral absorption and systemic availability.
Available Strengths and Dosage Forms
- Capsules in multiple strengths: 5 mg, 20 mg, 100 mg, 250 mg
- Injectable formulations in selected markets for intravenous use
Inactive Ingredients and Excipients
Temonat capsules contain excipients such as lactose, starch, and magnesium stearate. These aid in capsule integrity and bioavailability but have no pharmacological action.
Mechanism of Action: How Temozolomide Works
Classification as an Alkylating Agent
Temozolomide belongs to the alkylating agent group, interfering with DNA replication. It works by methylating DNA at specific sites, hindering cellular division and leading to tumor cell apoptosis.
DNA Methylation and Cytotoxic Effects on Tumor Cells
The drug methylates the O6 position of guanine residues in DNA. This triggers mismatched base-pairing and subsequent apoptosis in malignant cells, disrupting their proliferative capacity.
Selectivity for Rapidly Dividing Cancer Cells
Although normal cells can also be affected, rapidly dividing tumor cells are more vulnerable. This selective toxicity underpins Temozolomide’s therapeutic value in aggressive malignancies.
Pharmacokinetics and Metabolism
Temozolomide is rapidly absorbed after oral administration with almost complete bioavailability. It undergoes spontaneous hydrolysis to its active metabolite, MTIC (monomethyl triazeno imidazole carboxamide), which exerts the cytotoxic effect. Excretion is primarily renal.
Medical Uses of Temonat (FDA and Global Approvals)
Primary Indications and Approved Therapeutic Uses
- Treatment of glioblastoma multiforme (GBM)
- Management of anaplastic astrocytoma
Treatment of Glioblastoma Multiforme (GBM)
Temozolomide is approved as a first-line treatment in newly diagnosed GBM when combined with radiotherapy, followed by monotherapy. It prolongs progression-free and overall survival.
Anaplastic Astrocytoma Management
Temozolomide is used as monotherapy for recurrent anaplastic astrocytoma, offering clinical benefit where surgical and radiological interventions are limited.
Role in Newly Diagnosed Versus Recurrent Brain Tumors
In newly diagnosed cases, it is part of a combined regimen. In recurrent cases, Temozolomide provides therapeutic salvage when standard treatment options fail.
Off-Label Uses of Temozolomide
Use in Metastatic Melanoma
Temozolomide has shown modest benefit in advanced melanoma, particularly in patients with brain metastases due to its ability to cross the blood-brain barrier.
Neuroendocrine Tumors and Pituitary Carcinomas
Studies highlight its off-label application in resistant pituitary carcinomas and aggressive neuroendocrine tumors with variable outcomes.
Soft Tissue Sarcomas
Temozolomide is occasionally employed in investigational regimens for sarcomas, though its efficacy remains under evaluation.
Pediatric Oncology Applications
In pediatric neuro-oncology, Temozolomide has been explored in medulloblastomas and ependymomas, though safety and long-term outcomes warrant further study.
Emerging Research in Hematologic Malignancies
Early-phase clinical trials are evaluating its role in certain leukemias and lymphomas, particularly in refractory cases.
Dosage and Administration Guidelines
Standard Dosing Regimens for Glioblastoma and Astrocytoma
Typical dosing involves 150–200 mg/m² once daily for 5 days in a 28-day cycle, adjusted based on response and tolerance.
Cycle-Based Dosing Schedules
Treatment is structured into cycles, permitting bone marrow recovery and minimizing cumulative toxicity.
Oral Versus Intravenous Administration
Oral capsules are most common, while intravenous infusion is reserved for patients unable to take oral medication.
Dosage Adjustments in Renal and Hepatic Impairment
Patients with mild renal or hepatic impairment generally do not require adjustments, though caution is mandatory. Severe dysfunction may necessitate modifications.
Missed Dose Instructions
If a dose is missed, it should not be doubled. Patients are advised to consult their physician for corrective measures.
Side Effects of Temonat
Overview of Toxicity Profile and Tolerability
Temozolomide is generally tolerable but has predictable dose-limiting toxicities, especially affecting the hematopoietic system.
Hematologic Side Effects
- Anemia
- Leukopenia
- Thrombocytopenia
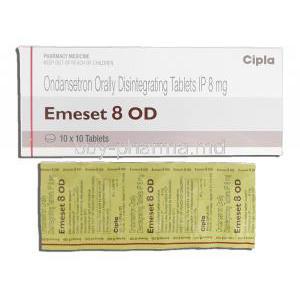
Gastrointestinal Disturbances
- Nausea
- Vomiting
- Constipation
- Diarrhea
Neurological Side Effects
- Headache
- Fatigue
- Seizures in predisposed patients
Common Side Effects
- Nausea and vomiting
- Loss of appetite
- Hair thinning
- Skin rash
- Constipation
- Headache
Serious and Rare Adverse Reactions
- Severe myelosuppression and pancytopenia
- Opportunistic infections such as Pneumocystis pneumonia
- Liver toxicity and hepatotoxicity
- Secondary malignancies due to prolonged DNA damage
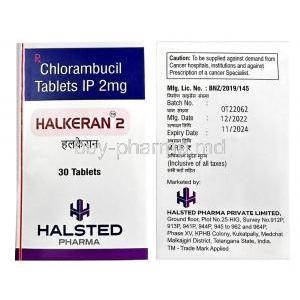
Drug Interactions with Temozolomide
Interactions with Other Chemotherapy Agents
Concurrent use with other alkylating drugs increases hematologic toxicity. Combination regimens must be closely monitored.
Effect of Corticosteroids and Antiemetics
Corticosteroids reduce inflammation but elevate infection risk when combined with Temozolomide. Antiemetics are often prescribed to mitigate nausea without significant interaction.
Risk of Infection with Immunosuppressants
Immunosuppressive drugs heighten the risk of opportunistic infections, necessitating vigilant monitoring.
Alcohol and Hepatotoxic Risk
Alcohol consumption amplifies hepatic burden, raising the potential for liver injury during Temozolomide therapy.
Interaction with Antiepileptic Drugs
Patients with brain tumors often require antiepileptics. Certain enzyme-inducing antiepileptics can alter Temozolomide metabolism, reducing effectiveness or heightening toxicity.
Contraindications
Known Hypersensitivity to Temozolomide or Dacarbazine
Temozolomide is contraindicated in patients with a history of hypersensitivity to the active substance or to dacarbazine, a related alkylating agent. Hypersensitivity reactions may include severe rashes, bronchospasm, and even anaphylaxis. Such patients must avoid exposure due to the risk of life-threatening complications.
Severe Myelosuppression at Baseline
Individuals with pre-existing severe bone marrow suppression must not initiate Temozolomide therapy. Profound reductions in white blood cells or platelets compromise immunity and increase hemorrhagic risks, making treatment unsafe until hematologic recovery is established.
Pregnancy and Breastfeeding Restrictions
Temozolomide demonstrates teratogenicity in animal studies and is strictly contraindicated during pregnancy. Exposure may lead to congenital malformations or fetal loss. Likewise, breastfeeding is prohibited, as excretion into human milk and subsequent neonatal harm cannot be excluded.
Warnings and Important Precautions
Monitoring Blood Counts During Therapy
Frequent monitoring of complete blood counts (CBC) is essential. Temozolomide can induce profound neutropenia and thrombocytopenia, warranting timely dose modifications or interruptions to mitigate risk.
Infection Risk and Prophylaxis Considerations
Patients with prolonged lymphopenia are predisposed to opportunistic infections. Prophylactic antibiotics, such as those used against Pneumocystis jirovecii pneumonia, may be necessary, especially in combination regimens with radiotherapy.
Hepatic and Renal Function Monitoring
Liver enzymes and renal parameters should be periodically assessed. Hepatotoxicity and renal impairment can exacerbate toxicity, making laboratory surveillance indispensable during prolonged therapy.
Long-Term Risk of Secondary Cancers
As with many alkylating agents, long-term administration carries a rare but notable risk of therapy-related leukemia and secondary malignancies. This necessitates vigilant follow-up even after discontinuation of therapy.
Risk of Pulmonary Toxicity
Rare cases of interstitial pneumonitis and pulmonary fibrosis have been reported. Patients presenting with unexplained cough or dyspnea should undergo prompt respiratory evaluation to exclude drug-induced lung injury.
Careful Administration in Special Populations
Elderly Patients
Elderly individuals often exhibit increased susceptibility to myelosuppression. Age-related decline in marrow reserve demands careful dose titration and intensified hematologic monitoring.
- Lower starting doses may be considered in frail patients.
- Routine blood count checks should be more frequent than in younger populations.
Pregnant and Nursing Women
Temozolomide poses significant teratogenic and embryotoxic risks. Women of childbearing potential should employ reliable contraception during therapy and for at least six months following cessation. Male patients are also advised to use contraception, given the mutagenic potential of the drug.
- Breastfeeding is strictly contraindicated throughout therapy.
- Pregnant women should not be exposed to Temozolomide handling due to teratogenic risk.
Pediatric Patients
Temozolomide has been utilized in children with malignant gliomas and other refractory brain tumors. While it shows therapeutic benefit, data on long-term safety remain limited. Dosing is calculated according to body surface area to optimize therapeutic efficacy while minimizing toxicity.
Overdosage and Emergency Management
Symptoms of Temozolomide Overdose
Excessive intake may manifest as severe bone marrow suppression, profound pancytopenia, and intractable gastrointestinal disturbances such as vomiting and diarrhea. Neurological symptoms, including seizures, may also arise in extreme overdose cases.
Supportive Care and Hospitalization
There is no specific antidote for Temozolomide overdose. Management relies on aggressive supportive care, hospitalization, and treatment in specialized oncology units.
Hematologic Recovery Strategies
Interventions may include transfusion support, administration of growth factors such as G-CSF, and protective isolation to reduce infection risk until hematologic parameters stabilize.
Handling and Safety Precautions
Safe Handling of Chemotherapy Capsules
Temozolomide capsules should be handled with caution. Caregivers are advised to wear gloves and avoid direct contact with capsule contents. In case of accidental spillage, thorough cleaning with protective equipment is mandatory.
Disposal of Unused Medication
Unused or expired medication should be disposed of according to local regulations for cytotoxic waste. Flushing into water systems or general household disposal is prohibited.
Protective Measures for Caregivers
Caregivers assisting patients must wash hands after handling medication and avoid exposure to contaminated excreta, as drug metabolites can be present in urine and vomit for several days after administration.
Storage Away from Heat, Light, and Moisture
Capsules must be kept in their original packaging at room temperature. Exposure to moisture or high heat can degrade the drug and reduce efficacy.
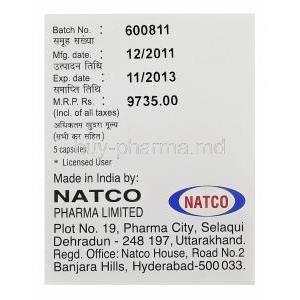
Storage and Shelf-Life
Recommended Storage Conditions
Store Temonat capsules at controlled room temperature, ideally below 25°C. They should be protected from direct sunlight and humidity.
Stability of Oral Capsules and Reconstituted Forms
Oral capsules remain stable when stored correctly until the manufacturer’s expiry date. Reconstituted or opened formulations, when available, have a limited shelf-life and require strict adherence to guidelines.
Expiry and Proper Disposal Guidelines
Expired medication must not be consumed. Disposal should follow institutional or pharmacy protocols for cytotoxic substances, ensuring environmental safety and preventing accidental exposure.
Temonat, Temozolomide FAQ
- What is temozolomide used for?
- What is the mechanism of action of temozolomide?
- How long can you stay on temozolomide?
- Do you lose your hair with temozolomide?
- How successful is temozolomide?
- What are the disadvantages of temozolomide?
- When is the best time to take temozolomide?
- Can temozolomide shrink glioblastoma?
- Do people only take temozolomide if their tumor is malignant?
- What to eat when taking temozolomide?
- Does temozolomide make you sleepy?
- What cancers is temozolomide used for?
- How toxic is temozolomide?
- Can you touch temozolomide?
- Why do you take temozolomide on an empty stomach?
- How quickly can a glioblastoma grow back?
- How soon can I eat after taking temozolomide?
- How bad is temozolomide?
- Does temozolomide cause cell death?
- Can you drink alcohol on temozolomide?
What is temozolomide used for?
Temozolomide is a type of chemotherapy. Doctors use it to treat brain tumours, particularly gliomas and anaplastic astrocytomas.
What is the mechanism of action of temozolomide?
Temozolomide works by altering the DNA of cells by adding a methyl group to the material. This happens after the drug is converted into its form called MTIC. The MTIC compound then targets the DNA attaching methyl groups to a spot, on the guanine molecule, known as the O6 position.
How long can you stay on temozolomide?
Up to 24 cycles
Do you lose your hair with temozolomide?
Yes
How successful is temozolomide?
56%
What are the disadvantages of temozolomide?
Temozolomide can lower white blood cells, thereby increasing the possibility of an infection.
When is the best time to take temozolomide?
Before any meal
Can temozolomide shrink glioblastoma?
Yes
Do people only take temozolomide if their tumor is malignant?
Temozolomide has shown promise as an effective treatment for gliomas, offering a new option for patients with this condition.
What to eat when taking temozolomide?
To take your medication, simply swallow the capsule or capsules whole with a glass of water. Don't try to crush or open them. Taking temozolomide when your stomach is empty tends to work better.
Does temozolomide make you sleepy?
Yes
What cancers is temozolomide used for?
Temozolomide, a medication commonly known as TMZ, has been approved for treating adults with certain types of brain tumors. Specifically, its approved for patients with astrocytoma, a grade III tumor, or glioblastoma, a more severe grade IV tumor.
How toxic is temozolomide?
Temozolomide's biggest downfall is its tendency to cause myelosuppression, a condition where the body's ability to produce blood cells is severely impaired.
Can you touch temozolomide?
No
Why do you take temozolomide on an empty stomach?
Taking this on an empty stomach, might help ease any queasiness and also seems to get absorbed.
How quickly can a glioblastoma grow back?
Generally, tumors of this type tend to recur within half a year to three quarters of a year after the initial diagnosis and treatment have taken place.
How soon can I eat after taking temozolomide?
1 hour after taking the medicine
How bad is temozolomide?
This medicine can have some side effects, particularly affecting your lungs or breathing.
Does temozolomide cause cell death?
Yes
Can you drink alcohol on temozolomide?
No