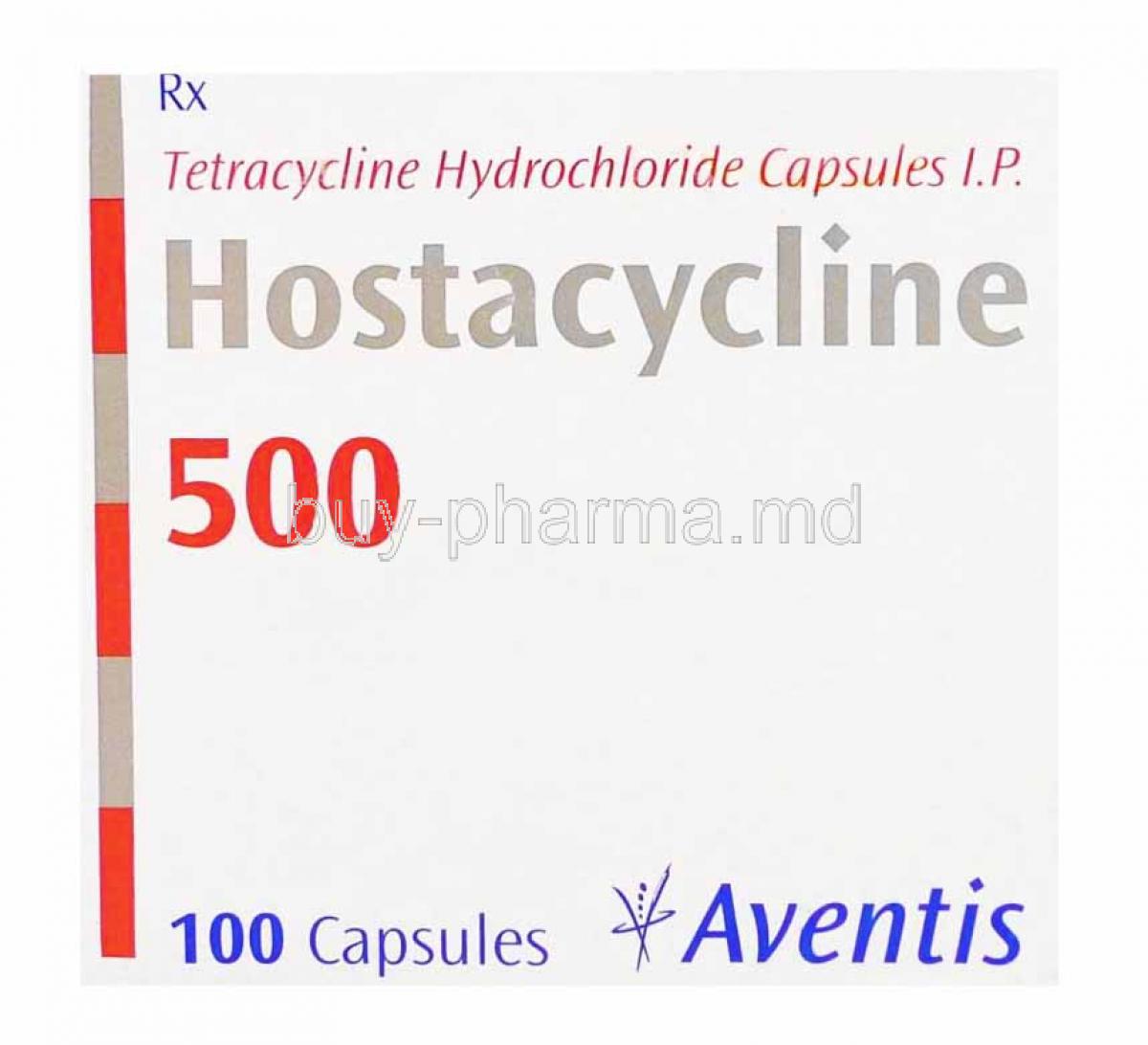
Introduction to Hostacycline (Tetracycline)
Overview of tetracycline antibiotics
Tetracyclines are broad-spectrum, bacteriostatic antibiotics that impede bacterial growth rather than outright destruction. Their utility spans community and hospital settings. Versatile. Time-tested.
- Class: Polyketide antibiotics derived from Streptomyces species
- Core effect: Suppress protein synthesis at the ribosomal level
- Coverage: Gram-positive, Gram-negative, atypicals, and select zoonotic pathogens
Historical background and medical significance
Introduced in the mid-20th century, tetracycline reshaped outpatient infection management by offering an oral, affordable, relatively safe option. Resistance patterns have evolved, yet the molecule retains importance in targeted indications and combination regimens.
Role of Hostacycline in infectious disease treatment
Hostacycline (tetracycline hydrochloride) remains relevant where susceptibility is demonstrated, as adjunctive therapy in specific syndromes, and in dermatologic and gastrointestinal protocols. Clinicians leverage it when first-line alternatives are unsuitable or contraindicated.
Composition and Formulation of Hostacycline
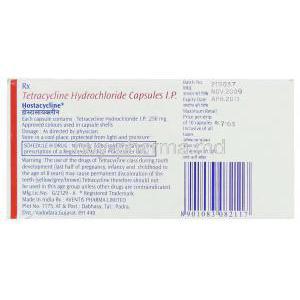
Active ingredient: Tetracycline hydrochloride
Each unit contains tetracycline hydrochloride, a semi-synthetic derivative optimized for oral bioavailability.
Available dosage forms: capsules, tablets, oral suspension
- Capsules/Tablets: Common strengths enabling 4-times-daily schedules
- Oral suspension: Useful where swallowing solid dosage forms is problematic
Excipients and inactive ingredients
Formulations typically include fillers (e.g., lactose or cellulose), disintegrants, and stabilizers. Exact excipient profiles vary by manufacturer; verify for allergy and dietary considerations.
Mechanism of Action: How Hostacycline Works
Inhibition of bacterial protein synthesis
Tetracycline reversibly binds the 30S ribosomal subunit, blocking aminoacyl-tRNA docking at the A-site. Translation stalls. Protein synthesis halts. The organism’s replication slows, enabling host defenses to eradicate infection.
Activity against Gram-positive and Gram-negative bacteria
- Gram-positive: Staphylococcus (susceptible strains), Streptococcus spp. (variable)
- Gram-negative: Haemophilus, Vibrio cholerae, select enterics (where susceptibility confirmed)
- Atypicals/others: Chlamydia, Mycoplasma, Rickettsia, spirochetes, and certain protozoa (as adjunct)
Bacteriostatic vs. bactericidal effects
Primarily bacteriostatic at standard doses. Bactericidal activity may occur against highly susceptible organisms at elevated concentrations, but this is not the clinical expectation.
Spectrum of antimicrobial activity
Broad, yet tempered by regional resistance. Culture and susceptibility data guide rational use, particularly for urogenital and respiratory pathogens with known resistance mechanisms.
Medical Uses of Hostacycline (Approved Indications)
Treatment of respiratory tract infections (pneumonia, bronchitis)
Considered when pathogens are susceptible and macrolide or beta-lactam options are unsuitable. Atypical coverage adds value in mixed etiologies.
Skin and soft tissue infections (acne vulgaris, cellulitis)
- Acne vulgaris: Anti-inflammatory and antimicrobial effects; commonly used in stepwise dermatologic regimens.
- Cellulitis: Only when likely organisms are susceptible and local resistance is low.
Genitourinary infections (chlamydia, gonorrhea, syphilis)
Utility is pathogen- and region-specific. For Chlamydia trachomatis and certain spirochetal infections, tetracycline may be used where guidelines permit and susceptibility is documented. Gonorrhea management generally requires alternative agents due to resistance; use only if susceptible strains are confirmed.
Gastrointestinal infections (cholera, Helicobacter pylori-related gastritis)
- Cholera: Effective against V. cholerae to reduce stool volume and disease duration.
- H. pylori: A component of bismuth-based quadruple therapy in eradication regimens.
Rickettsial infections (Rocky Mountain spotted fever, typhus, Q fever)
Alternative when preferred agents are unavailable or contraindicated; activity extends across multiple rickettsioses.
Zoonotic infections (brucellosis, plague, anthrax, tularemia)
Applied as part of combination therapy or post-exposure protocols, contingent on susceptibility and public health guidance.
Eye infections (trachoma, conjunctivitis caused by susceptible organisms)
Systemic therapy may be employed in trachoma control strategies alongside hygienic measures and, where indicated, topical therapy.
Off-Label and Specialized Uses
Malaria prophylaxis and treatment
Historical and adjunctive role. Used with other antimalarials where local resistance and guideline frameworks justify inclusion.
Periodontal disease management
Low-dose regimens may modulate matrix metalloproteinases, improving periodontal outcomes when combined with mechanical debridement.
Lyme disease and other tick-borne infections
An alternative in specific scenarios when first-line therapy is unsuitable, with attention to disease stage and local resistance patterns.
Rosacea and inflammatory skin conditions
Anti-inflammatory effects can attenuate papulopustular activity and erythema; dermatologists may deploy short-course or pulsed regimens.
Multidrug-resistant bacterial infections (as combination therapy)
Strategic, susceptibility-driven use in combination protocols to leverage synergistic effects and reduce resistance emergence.
Dosage and Administration Guidelines
Standard adult dosage recommendations
- Typical infections: 250–500 mg every 6 hours (total 1–2 g/day), based on severity and site.
- Acne: often 250 mg 2–4 times daily initially, then titrated to the lowest effective dose.
- Cholera: regimen varies by guideline; multi-day courses commonly used where susceptibility persists.
- H. pylori eradication: 500 mg four times daily within bismuth-based quadruple therapy for 10–14 days.
Dosing should reflect current local guidelines and susceptibility data.
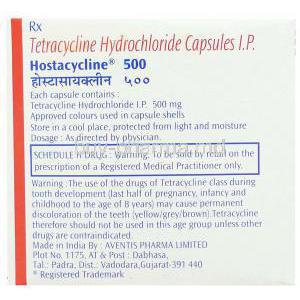
Pediatric dosing considerations
- Contraindicated in children <8 years due to permanent tooth discoloration and effects on bone growth, except for life-threatening infections when benefits outweigh risks.
- If used: 25–50 mg/kg/day divided every 6 hours (maximum typically 2 g/day), under specialist guidance.
Duration of therapy for different infections
- Respiratory/skin: commonly 7–14 days, tailored to clinical response.
- Acne/rosacea: weeks to months with periodic reassessment to minimize resistance.
- H. pylori: 10–14 days as part of combination therapy.
- Rickettsial illnesses: at least 7 days and until afebrile for 2–3 days, per protocol.
Administration with food or on an empty stomach
For optimal absorption, take on an empty stomach: 1 hour before or 2 hours after meals. Swallow with a full glass of water and remain upright for 30 minutes to reduce esophageal irritation.
- Avoid concurrent intake with dairy (milk, yogurt), calcium-fortified juices, iron, magnesium, zinc, aluminum-containing antacids.
- Separate chelating agents and supplements by at least 2–3 hours.
Missed dose instructions
- Take the missed dose as soon as remembered if it is not close to the next scheduled dose.
- If near the next dose, skip the missed dose—do not double up.
- Resume the regular schedule and complete the full course.
Dose adjustments in renal or hepatic impairment
Tetracycline is primarily renally eliminated. Accumulation can occur in significant renal dysfunction, increasing the risk of azotemia and other adverse effects.
- Renal impairment: Consider extended dosing intervals or reduced total daily dose; monitor BUN/creatinine and clinical status.
- Hepatic impairment: Use cautiously; avoid high doses and prolonged courses. Monitor liver enzymes during extended therapy.
- In severe organ dysfunction, evaluate alternative agents with safer pharmacokinetics when feasible.
Side Effects of Hostacycline
Common Side Effects
Hostacycline, like other tetracycline antibiotics, may cause mild to moderate side effects in some individuals. These reactions are often transient but can affect treatment adherence if not anticipated.
- Gastrointestinal disturbances: Nausea, vomiting, abdominal discomfort, and diarrhea are frequently reported due to irritation of the gastrointestinal mucosa.
- Photosensitivity and skin rash: Sunburn-like reactions can develop with even limited sun exposure, often accompanied by erythematous skin rash.
- Tooth discoloration and enamel hypoplasia: In children and during tooth development, tetracyclines can cause permanent yellow-brown discoloration and structural weakening of enamel.
- Headache and dizziness: Neurological effects are less common but may impair concentration and daily activities in susceptible patients.
Serious Adverse Reactions
Though uncommon, certain adverse events require immediate medical evaluation due to their potential severity.
- Hepatotoxicity: Elevated liver enzymes, hepatitis, or hepatic dysfunction may occur, particularly with high or prolonged dosing.
- Hypersensitivity reactions: Urticaria, angioedema, or anaphylaxis can develop suddenly and may be life-threatening if untreated.
- Intracranial hypertension: Characterized by severe headache, blurred vision, and papilledema, this rare complication has been observed in adults and adolescents.
- Blood disorders: Cases of hemolytic anemia, leukopenia, and thrombocytopenia have been documented, requiring careful hematologic monitoring in long-term therapy.
Drug Interactions with Hostacycline
The therapeutic efficacy of Hostacycline can be compromised or altered by interactions with certain foods and medications.
- Dairy products and calcium-rich foods: Calcium binds tetracycline, reducing gastrointestinal absorption and decreasing plasma concentrations.
- Iron, magnesium, and antacids: Chelation with divalent or trivalent cations prevents proper absorption, leading to therapeutic failure if co-administered.
- Oral contraceptives: Tetracyclines may decrease contraceptive efficacy, increasing the risk of breakthrough pregnancy.
- Anticoagulants and antidiabetic medications: Hostacycline may potentiate anticoagulant effects and alter glucose control, necessitating dose adjustments.
- Retinoids and methoxyflurane: Concomitant use can increase the risk of intracranial hypertension or renal toxicity, respectively.
Warnings and Precautions
Prudent use of Hostacycline ensures effectiveness while minimizing risks associated with misuse or inappropriate administration.
- Completing therapy: Full adherence to prescribed duration prevents relapse and reduces the risk of resistant bacterial strains.
- Resistance development: Overuse or premature discontinuation encourages microbial resistance, complicating future treatments.
- Photosensitivity precautions: Patients should avoid excessive sun exposure, use sunscreen, and wear protective clothing.
- Organ function monitoring: Liver and kidney function should be periodically assessed during extended therapy courses.
Contraindications
Certain populations and conditions preclude the safe use of Hostacycline.
- Hypersensitivity: Contraindicated in individuals with known allergy to tetracyclines.
- Pediatric use: Children under 8 years should not receive therapy except in life-threatening cases due to risks to teeth and bones.
- Severe hepatic impairment: Risk of hepatotoxicity is significantly amplified.
- Concurrent isotretinoin use: Increases the likelihood of intracranial hypertension.
Careful Administration in Special Populations
Elderly Patients
Elderly individuals often exhibit reduced renal clearance, necessitating dosage adjustments. Close observation for hepatotoxicity is recommended due to age-related physiological decline.
Pregnant and Nursing Women
Tetracyclines cross the placenta and can impair fetal skeletal development, rendering Hostacycline contraindicated during pregnancy. Excretion in breast milk exposes infants to tooth discoloration and bone effects, making breastfeeding incompatible with treatment.
Pediatric Patients
Routine administration is not advised under 8 years of age. However, in critical infections such as rickettsial diseases or inhalational anthrax, physicians may authorize use when benefits outweigh risks.
Overdosage and Emergency Management
Excessive ingestion may lead to toxic manifestations requiring immediate medical intervention.
- Symptoms: Severe nausea, vomiting, hepatotoxicity, renal impairment, and neurological effects may present.
- Supportive treatment: Hydration, electrolyte management, and monitoring of vital signs form the cornerstone of care.
- Gastric lavage and activated charcoal: May be employed if ingestion is recent.
- Laboratory monitoring: Renal and hepatic function should be closely observed until stabilization occurs.
Storage and Handling Precautions
Correct storage and handling preserve drug potency and prevent accidental misuse.
- Storage conditions: Maintain in a cool, dry environment away from direct sunlight and excessive humidity.
- Shelf-life: Observe expiration dates, as degraded tetracyclines may cause renal toxicity.
- Safe disposal: Discard expired or unused medication responsibly, avoiding household waste or wastewater systems.
- Healthcare provider precautions: Handle with care to avoid accidental exposure; maintain appropriate hygiene protocols.