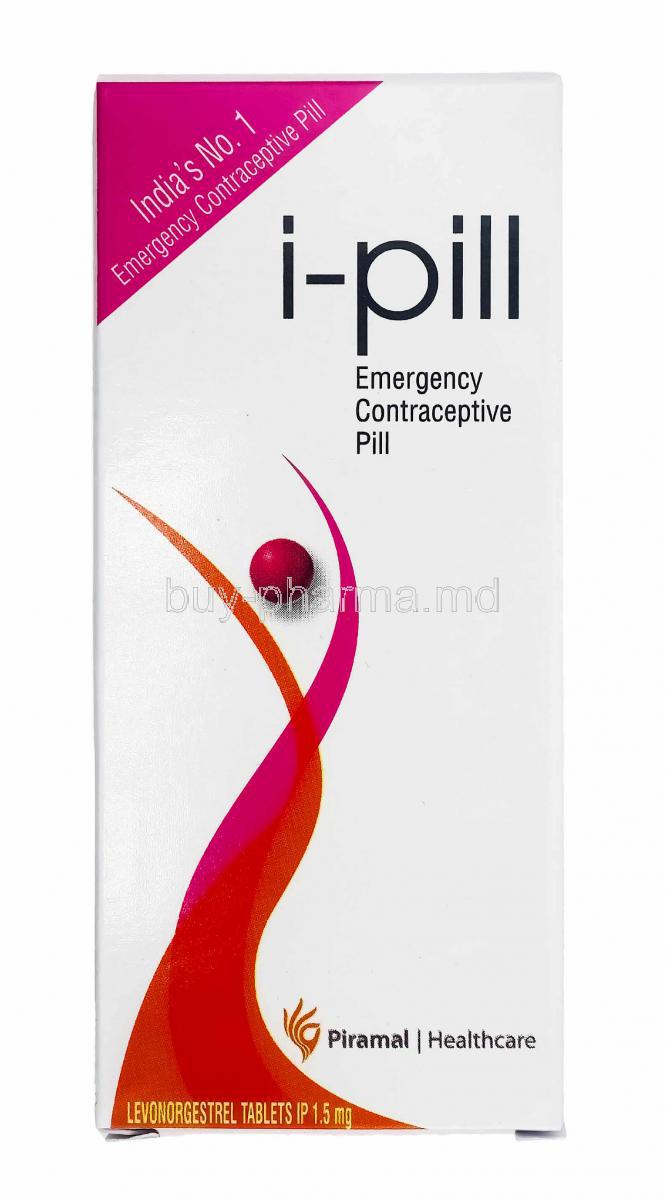
i-Pill, Levonorgestrel
- Introduction
- Composition
- Active Ingredient: Levonorgestrel
- Inactive Ingredients and Excipients
- Available Strengths and Dosage Forms
- Levonorgestrel and Ethinyl Estradiol
- Levonorgestrel vs Norethindrone
- Levonorgestrel vs Progesterone
- Norgestrel vs Levonorgestrel
- Norethindrone vs Levonorgestrel
- Ethinylestradiol Levonorgestrel
- Levonorgestrel vs Norgestrel
- Etonogestrel vs Levonorgestrel
- Drospirenone vs Levonorgestrel
- Levonorgestrel vs Etinilestradiol
- Norgestimate vs Levonorgestrel
- Desogestrel vs Levonorgestrel
- Levonorgestrel vs Drospirenone
- Levonorgestrel vs Etonogestrel
- Levonorgestrel vs Plan B
- Norethindrone Acetate vs Levonorgestrel
- Aviane Levonorgestrel and Ethinyl Estradiol
- How i-Pill Works
- Uses of i-Pill (Levonorgestrel)
- Off-Label Uses of Levonorgestrel
- Dosage and Administration
- Administration in Special Populations
- Common Side Effects
- Possible Side Effects and Adverse Reactions
- Overdosage
- Drug Interactions
- Warnings and Precautions
- Levonorgestrel Contraindications
- Careful Administration
- Important Precautions
- Handling and Storage
Introduction
Contemporary reproductive healthcare relies heavily on emergency contraception (EC). The i-Pill, which contains the synthetic progestogen levonorgestrel, is a leading example. This single-dose formulation has revolutionized the global conversation about post-coital birth control, largely due to its high accessibility and proven effectiveness in preventing unintended pregnancies across diverse populations.
Levonorgestrel works by delaying or stopping ovulation, but its success is highly time-sensitive: it must be taken as soon as possible after unprotected intercourse, and no later than 72 hours. This importance is underscored by its global use (over 100 countries) and its status as an essential medicine by the World Health Organization (WHO). Patients should receive counseling about its potential side effect of temporarily altering the menstrual cycle (e.g., earlier, later, or heavier bleeding).
Composition
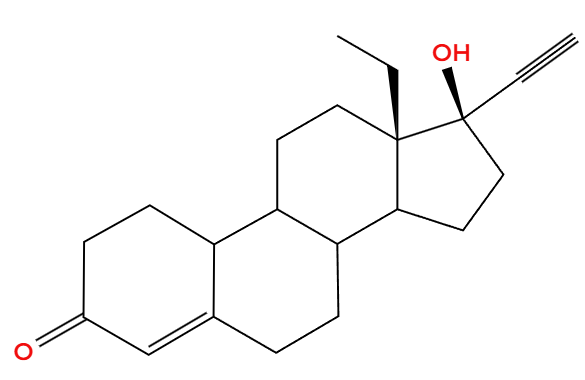
Active Ingredient: Levonorgestrel
Levonorgestrel is a synthetic progestin of the second generation. It primarily works by inhibiting ovulation and thickening the cervical mucus. Its pharmacological strength and positive safety profile set it apart from earlier agents.
Inactive Ingredients and Excipients
Formulations frequently incorporate excipients like lactose monohydrate, maize starch, magnesium stearate, and colloidal silicon dioxide. Although these substances are clinically inactive, they play a significant role in affecting tablet stability, absorption kinetics, and shelf life.
Available Strengths and Dosage Forms
The i-Pill typically contains 1.5 mg of levonorgestrel in a single oral tablet. In some markets, 0.75 mg tablets are available, which should be taken twice within 12 hours. Prolonged use of combined oral contraceptives containing levonorgestrel and ethinyl estradiol expands its range of applications.
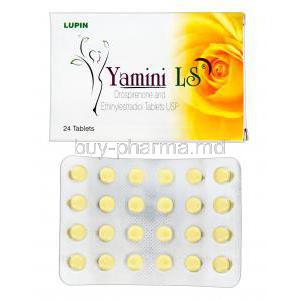
Levonorgestrel and Ethinyl Estradiol
This combination establishes the basis for many combined oral contraceptives. Ethinyl estradiol improves cycle regulation, while levonorgestrel guarantees contraceptive reliability. Together, they strike a balance between efficacy and tolerability.
Levonorgestrel vs Norethindrone
Norethindrone, a first-generation progestin, provides contraceptive advantages but has a slightly reduced progestational profile compared to levonorgestrel. Levonorgestrel exhibits greater receptor affinity, which results in improved potency at lower doses.
Levonorgestrel vs Progesterone
Progesterone is a natural hormone produced by the body, crucial for maintaining pregnancy. Levonorgestrel, a synthetic version, replicates its effects but is available in oral form, more stable, and better suited for contraceptive products.
Norgestrel vs Levonorgestrel
Norgestrel is a racemic mixture. Levonorgestrel is the active enantiomer, offering enhanced pharmacodynamic efficiency. Consequently, levonorgestrel provides similar effectiveness with lower dosing requirements.
Norethindrone vs Levonorgestrel
Both are oral progestins, but levonorgestrel is viewed as more potent. Norethindrone carries extra androgenic effects, sometimes resulting in acne or weight changes, which are not as noticeable with levonorgestrel.
Ethinylestradiol Levonorgestrel
This combination supports numerous monophasic and triphasic contraceptives. Ethinylestradiol promotes cycle regularity, while levonorgestrel sustains contraceptive effectiveness. The pairing has been thoroughly researched, showing consistent efficacy rates surpassing 99% with ideal use.

Levonorgestrel vs Norgestrel
Pharmacological nuance emphasizes levonorgestrel as the active isomer of norgestrel. This distinction enables lower doses to reach therapeutic equivalence.
Etonogestrel vs Levonorgestrel
Etonogestrel is commonly utilized in subdermal implants, offering long-lasting contraception. Levonorgestrel is adaptable, found in pills, intrauterine devices, and as emergency contraception. Both substances are highly effective, yet they vary in their delivery methods and length of action.
Drospirenone vs Levonorgestrel
Drospirenone, a more recent progestin, shows anti-mineralocorticoid effects, helping to lessen bloating and fluid retention. In comparison, levonorgestrel focuses on its effectiveness and broad clinical application, with minimal issues related to electrolyte imbalances.
Levonorgestrel vs Etinilestradiol
In Spanish-speaking nations, this combination of levonorgestrel vs ethinilestradiol to be a widely accepted as a contraceptive method. Clinical results are consistent with global observations: dependable pregnancy prevention paired with a strong record of safety.
Norgestimate vs Levonorgestrel
Norgestimate is less androgenic and is frequently favored for patients who are susceptible to acne or seborrhea. Levonorgestrel, on the other hand, continues to be a cornerstone because of its strong efficacy and well-established pharmacokinetic profile.

Desogestrel vs Levonorgestrel
Desogestrel is frequently used in progestin-only pills and has a lower androgenic index. Levonorgestrel is more powerful but somewhat more androgenic, affecting prescriber decisions according to patient requirements.
Levonorgestrel vs Drospirenone
While levonorgestrel focuses on effective ovulation suppression, drospirenone offers extra advantages such as enhanced fluid balance and mood stabilization for certain patients. The clinical situation determines the selection.
Levonorgestrel vs Etonogestrel
Both agents effectively inhibit ovulation. Etonogestrel’s implant offers a consistent long-term release, while levonorgestrel delivers quick post-coital intervention or prolonged action in intrauterine devices.
Levonorgestrel vs Plan B
Plan B is basically a branded version of levonorgestrel emergency contraception. The two are chemically the same; the differences mainly come down to branding and distribution.
Norethindrone Acetate vs Levonorgestrel
Norethindrone acetate is often used to address abnormal uterine bleeding and endometriosis. Levonorgestrel, on the other hand, leads the contraceptive market, especially in emergency and long-acting intrauterine products.
Aviane Levonorgestrel and Ethinyl Estradiol
Aviane is a commonly prescribed low-dose combined oral contraceptive that includes 20 mcg of ethinyl estradiol and 100 mcg of levonorgestrel. The reduced estrogen level helps to limit adverse effects while ensuring effective contraception.
How i-Pill Works
Mechanism of Action in Preventing Pregnancy
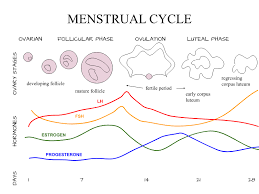
The i-Pill works due to its active ingredient, levonorgestrel, a potent synthetic progestin. Its main strategy is to prevent or delay ovulation by suppressing the surge of luteinizing hormone (LH). This action removes the egg as a potential target for sperm, virtually eliminating the chance of fertilization.
If ovulation is already underway, levonorgestrel provides two secondary safeguards:
- It alters cervical mucus, making it thicker and impeding sperm from traveling up the reproductive tract.
- It reduces the uterus's lining receptivity, making it harder for a fertilized egg (if one formed) to implant.
This rapid, biochemical, and time-sensitive approach is what makes it a comprehensive and effective emergency contraceptive when used promptly.
Effects on Ovulation, Fertilization, and Implantation
Levonorgestrel creates a complex, multi-stage barrier to prevent pregnancy. Its effectiveness depends on when it's taken:
- Before Ovulation: It stops the follicle from rupturing, preventing the egg from being released.
- Around Ovulation: It slows sperm movement by thickening cervical mucus and changes how the egg and sperm travel within the fallopian tubes.
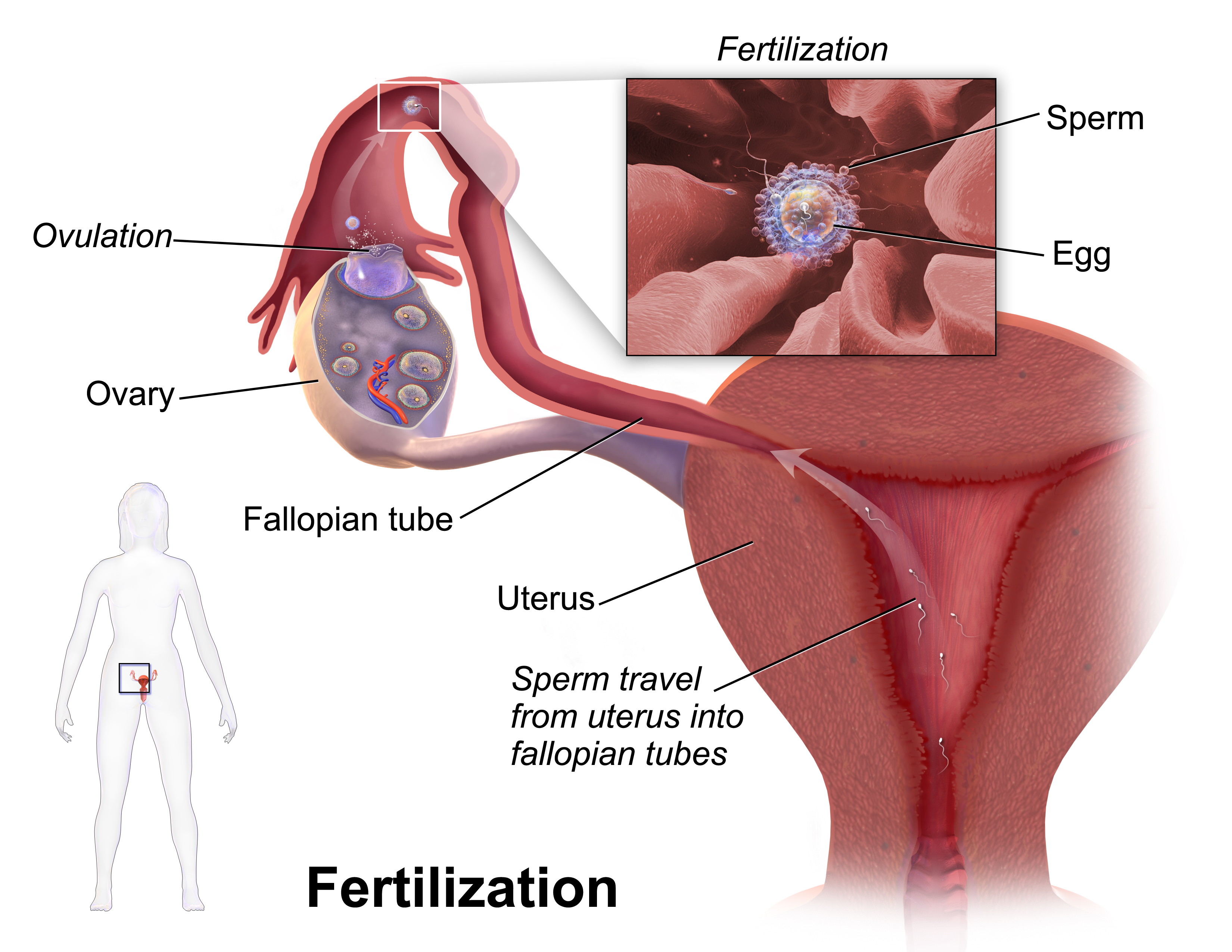
- After Fertilization: It alters the lining of the uterus (endometrium), making implantation of a fertilized egg highly unlikely.
By disrupting multiple stages of the reproductive process, levonorgestrel effectively prevents conception. Crucially, the pill does not work once implantation has already happened, which distinguishes emergency contraception from methods that induce abortion.
Differences from Regular Oral Contraceptives
The key difference between regular birth control pills and the i-Pill is their purpose. Standard oral contraceptives are taken daily to provide continuous, long-term pregnancy prevention by maintaining steady hormone levels. They also offer benefits like cycle regulation and reduced menstrual pain.
In contrast, the i-Pill is a single-use emergency solution taken after unprotected sex or contraceptive failure. It contains a much higher dose of only levonorgestrel (unlike regular pills that often combine estrogen and progestin) and does not provide the cycle-regulating benefits. Therefore, the i-Pill must be understood as a contingency measure, not a substitute for routine, daily birth control.
Levonorgestrel Interactions
The effectiveness of levonorgestrel can be compromised by certain medications. Specifically, drugs and herbal supplements (like St. John's Wort) that speed up the liver's metabolism (by inducing cytochrome P450 enzymes) can lower the concentration of levonorgestrel in the blood, thereby reducing its efficacy as an emergency contraceptive.
Examples of these "enzyme inducers" include drugs used for epilepsy (e.g., phenytoin, carbamazepine), tuberculosis (rifampicin), and some HIV treatments. When a patient is taking these substances, healthcare providers may need to recommend alternative or additional contraceptive methods. Apart from these specific drug interactions, levonorgestrel is generally safe and minimally interferes with most other medications. Knowing these specific interactions is vital for ensuring reliable protection.
Uses of i-Pill (Levonorgestrel)
Primary Use as Emergency Contraception
The i-Pill offers quick, single-dose contraception following unprotected sex, but it is intended only for emergency use, not as a regular daily birth control method. Its effectiveness is highly time-dependent: it must be taken as soon as possible to interrupt the process of ovulation.
- It works best when taken within 24 hours.
- It is usable up to 72 hours, though its efficacy significantly decreases after that point.
- It is not an abortifacient as it cannot end an established pregnancy.
In summary, the i-Pill is a time-bound, contingency measure, serving as a backup when routine contraception fails or is missed.
Levonorgestrel Delay Period
After taking emergency contraception, the timing of the next period may change. Many women experience a slight delay, but the period could also arrive earlier. The nature of the flow may also be different, potentially being lighter, heavier, or involving spotting.
These changes are temporary, reflecting the pill's immediate impact on your hormones, not a long-term cycle problem. You should generally expect your period within seven days of its usual date. If your period is delayed by more than one week, it is important to take a pregnancy test. Note that some intermittent spotting is common 2 to 7 days after taking the pill.
Levonorgestrel and Ethinyl Estradiol for Irregular Periods
Combined oral contraceptives (COCs), which contain both levonorgestrel (a progestin) and ethinyl estradiol (an estrogen), are frequently prescribed to regulate erratic menstrual cycles. The estrogen component stabilizes the uterine lining (endometrium), while the progestin prevents ovulation, resulting in predictable, scheduled withdrawal bleeding.
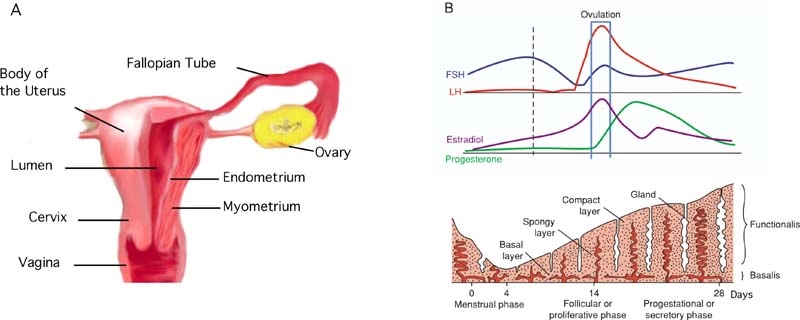
These pills offer several benefits, including achieving cycle regularity, reducing menstrual pain (dysmenorrhea), and easing heavy bleeding (menorrhagia). Crucially, COCs are not the same as emergency contraception because their purpose and dosing are entirely different. When selecting a method, practitioners must consider the patient's preferences, metabolic health, and any reasons to avoid estrogen. For severe heavy bleeding, a device like the levonorgestrel intrauterine system (IUS) is another option.
Prevention of Unintended Pregnancy After Unprotected Intercourse
The primary goal of levonorgestrel is to immediately reduce the risk of pregnancy following contraceptive failure or unprotected sex. It achieves this by delaying or blocking ovulation and thickening cervical mucus to impede sperm, thereby decreasing the likelihood of fertilization during the fertile window.
Its efficacy is highly time-dependent: it works best when taken within 24 hours and is only effective up to 72 hours. Patients should be aware that other options exist with longer windows of efficacy, such as the copper IUD (up to five days) or ulipristal acetate (up to 120 hours). Furthermore, individuals with a higher body weight may experience reduced effectiveness and should be counseled on alternative emergency methods.
Situations Warranting Use (Condom Failure, Missed Pills, Forced Intercourse)
Emergency contraception (EC) is necessary whenever a person has had unprotected sex or when their primary birth control method has failed. The goal is to intervene quickly and privately to reduce the chance of conception.
Situations warranting EC include:
- Barrier failure (like a condom breaking or slipping).
- Hormonal lapses (such as forgetting routine pills or delaying an injection).
- Unplanned exposure (using no method, or relying on withdrawal/coitus interruptus).
- It is a required component of post-sexual assault care.
- It is needed if a patient is taking enzyme-inducing drugs that reduce the effectiveness of their regular hormonal birth control.
Best practice dictates prompt access, clear guidance, and follow-up pregnancy testing if the next period is delayed.
Off-Label Uses of Levonorgestrel
Management of Heavy Menstrual Bleeding
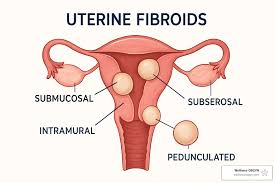
Levonorgestrel is highly effective in treating menorrhagia (abnormally heavy menstrual bleeding) when delivered through an intrauterine system (IUS). The IUS provides a localized dose that acts directly on the uterine lining (endometrium), significantly reducing the blood vessels and thickness of the tissue. This results in a substantial and often rapid decrease in menstrual blood loss.
This therapeutic approach greatly improves the patient's quality of life, preventing issues like chronic fatigue and anemia. It is a major alternative to more invasive surgical options for heavy bleeding, such as a hysterectomy or endometrial ablation, and can decrease the need for such procedures.
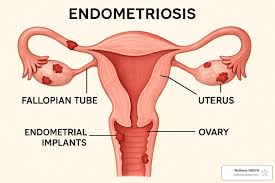
Hormonal Therapy in Endometriosis
Levonorgestrel is an effective treatment for endometriosis, a condition causing severe pain and infertility due to the growth of uterine lining tissue outside the uterus. Levonorgestrel works by using its anti-inflammatory and antiproliferative qualities to lessen the cyclical growth of these misplaced tissue implants.
By reducing the estrogen-driven function of the uterine lining, levonorgestrel-based therapies significantly relieve pelvic pain and painful periods (dysmenorrhea). When administered through an intrauterine device (IUD), it offers localized suppression, causing the tissue implants to shrink (atrophy). While not a cure, this approach helps manage symptoms, reduces reliance on general painkillers, and provides a valuable alternative or addition to surgery for many patients.
Potential Role in Polycystic Ovary Syndrome (PCOS)
Polycystic Ovary Syndrome (PCOS) is a complex hormonal condition defined by the lack of ovulation, excess male hormones (hyperandrogenism), and metabolic issues. To manage this, levonorgestrel, usually combined with ethinyl estradiol (estrogen), is used to regulate the menstrual cycle.
This combined treatment helps to:
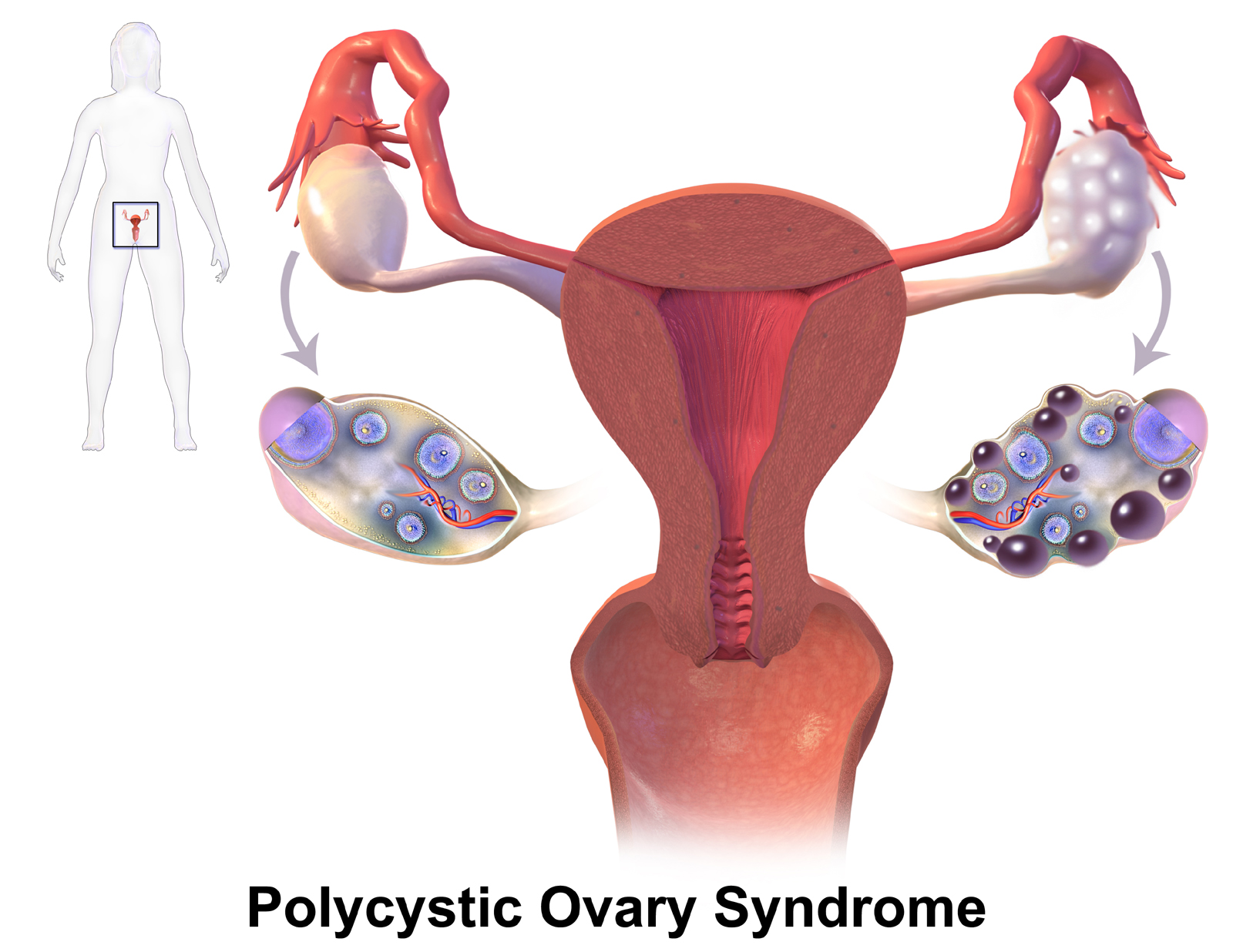
- Restore a predictable pattern of withdrawal bleeding.
- Reduce the risk of endometrial hyperplasia (thickening of the uterine lining) caused by chronic lack of ovulation.
- Bring about a hormonal balance that may also improve some androgen-related symptoms.
However, its use requires careful evaluation, especially for patients who have a high risk of cardiovascular or metabolic problems, where other hormonal therapies might be safer.
Use in Contraception Beyond Single-Dose Regimens
Levonorgestrel is used not just as emergency contraception, but also as a key component in long-term birth control strategies. Its versatile pharmacological properties are utilized in several highly effective forms of sustained contraception:
- Intrauterine Systems (IUS): Provide pregnancy prevention for up to five years.
- Combined Oral Pills: Taken daily to both prevent conception and regulate menstrual cycles.
- Subdermal Implants: Deliver a steady, sustained systemic release of the hormone.
These diverse, extended-use methods transform levonorgestrel from a one-time emergency solution into a cornerstone for sustained, everyday contraceptive care, demonstrating its broad applicability in meeting various reproductive needs.
Dosage and Administration
Levonorgestrel Dosage
For emergency contraception, levonorgestrel is typically taken as a single oral dose of 1.5 mg for a swift hormonal effect. While a split-dose regimen of two 0.75 mg tablets taken 12 hours apart is available in some areas, both methods provide comparable effectiveness. The simpler single-dose method is generally preferred because it makes it easier for patients to stick to the regimen (improving adherence). Notably, the drug is well-absorbed orally and its absorption is not affected by food.
Standard Recommended Dosage for Emergency Contraception
The most widely recommended way to take levonorgestrel for emergency contraception is a single 1.5 mg oral dose, which should be administered as soon as possible after unprotected intercourse to maximize effectiveness. While an alternative regimen exists (two 0.75 mg doses spaced 12 hours apart), the single-dose is preferred. It is important to note that the pill should not be repeated within the same menstrual cycle unless the user has another episode of high-risk sexual exposure.
Optimal Time Window for Effectiveness (Within 24â72 Hours)
The success of levonorgestrel as an emergency contraceptive is highly dependent on how quickly it is taken. The sooner it is administered, the better it prevents ovulation and conception.
- Its efficacy is maximal (around 95%) within the first 24 hours.
- Effectiveness is still strong but begins to decrease between 24 and 48 hours (around 85%).
- Effectiveness significantly drops between 48 and 72 hours (around 58%).
Because its power is markedly reduced after 72 hours, alternative methods, such as inserting a copper intrauterine device (IUD), should be considered.
Instructions for Missed or Delayed Doses
If the levonorgestrel dose is vomited within two hours of taking it, the user must immediately take another tablet. For those using the two-dose 0.75 mg regimen, delaying the second tablet past 16 hours may lessen its effectiveness; therefore, this dose should be completed right away. Remember not to exceed the recommended frequency within one menstrual cycle. If your next period is delayed by more than seven days, it is essential to get a pregnancy test.

Special Considerations in Repeated Use
While taking levonorgestrel more than once in the same cycle poses no major toxicity risk, it is not recommended as a routine practice. Repeated dosing can cause menstrual irregularities, such as unexpected bleeding or delayed periods, and generally disrupt the normal endocrine function, making cycles unpredictable. For anyone who finds themselves needing emergency contraception multiple times, the best course of action is to switch to a reliable, long-term method of contraception for greater stability and dependability.
Administration in Special Populations
Administration to Elderly Women
There is no reason to prescribe levonorgestrel to women who have reached menopause because their reproductive function has naturally ended. Furthermore, there is very little pharmacological data available concerning the effects of this drug in postmenopausal individuals.
Use in Pregnant Women and Nursing Mothers
Levonorgestrel should not be used if pregnancy is known (it is contraindicated) because it offers no benefit once implantation has occurred. While the drug has not been linked to birth defects (teratogenic effects) if exposure happens during pregnancy, it is still not recommended for routine use in pregnant individuals. For women who are breastfeeding, occasional use is considered safe, despite the fact that a small amount of the hormone has been found to pass into breast milk.
Levonorgestrel While Breastfeeding
Breastfeeding mothers can safely use levonorgestrel for emergency contraception with minimal risk to their infant. Only a small amount of the hormone transfers into the breast milk. As an optional precaution to further reduce the infant's exposure, mothers can choose to interrupt nursing for 3 to 4 hours immediately after taking the pill. The use of levonorgestrel has not been shown to negatively affect milk production.
Safety and Contraindications
- Safety: Safe for occasional emergency use during breastfeeding.
- Contraindications: None explicitly stated in this text, but the general context implies it's safe unless the mother wishes to reduce the minimal transfer by delaying feeding.

Safety in Children and Adolescents
Levonorgestrel is approved for use as emergency contraception in adolescents who have already started menstruating (post-menarcheal individuals). In this age group, its safety and effectiveness are comparable to those observed in adult women. However, it is crucial to provide thorough education and counseling to ensure adolescents understand how to use the pill correctly and to encourage them to adopt a standard, long-term contraceptive method rather than relying on emergency contraception regularly.
Considerations for Women with Liver or Kidney Impairment
Since the liver is the primary way the body metabolizes levonorgestrel, it is contraindicated (should be avoided) in women with severe liver disease.
For individuals with kidney issues:
- Mild to moderate renal impairment does not require a change in dosage, as it doesn't significantly affect the drug's clearance.
- More advanced kidney problems still require caution and medical supervision.
Mild liver dysfunction is not an absolute bar to treatment, and occasional emergency use may be permitted under a doctor's guidance. Ultimately, doctors must use clinical judgment to balance the drug's benefits against the risks of altered metabolism in any patient with compromised organ function.
Common Side Effects
Nausea and Vomiting
The most common reaction to levonorgestrel is transient gastrointestinal discomfort. Nausea is a frequent symptom that typically starts within a few hours and resolves naturally. Vomiting is rare, but a clinical concern because it can prevent the drug from being absorbed properly.
Symptoms usually start 2 to 8 hours after the dose. To manage them, it's advised to have light meals or ginger tea, and an anti-nausea medication (antiemetic) can be used if necessary. A key point is that if you vomit within two hours of taking the pill, you should typically take another dose.
It's also helpful to stay hydrated and get rest. If symptoms are severe or persist, you should seek medical attention to ensure they aren't caused by a different issue.
Irregular Bleeding or Spotting
After taking the emergency dose, it's common to experience breakthrough bleeding or spotting between periods. The effect on your next menstrual cycle is highly variable: your period could be earlier or delayed, and the flow might be lighter or heavier than usual. This spotting often occurs 2 to 7 days after taking the pill. These shifts are due to temporary changes in the uterine lining (endometrium) and are not a sign of permanent cycle disruption. If your period is delayed by more than 7 days, a pregnancy test is recommended. Normal cycle timing usually resumes with the period following the next one.
Fatigue and Dizziness
A small number of people report feelings of tiredness, lightheadedness, or a faint/vasovagal sensation. These effects are usually minor and go away on their own. If you feel severely dizzy, you should not drive or operate machinery. Make sure you stay well-hydrated and eat properly. Seek medical help immediately if you faint (syncope), experience ongoing vertigo, or notice any neurological changes.

Headache and Breast Tenderness
Headaches (cephalalgia) and breast tenderness (mastalgia) are possible side effects caused by temporary changes in hormone levels. This discomfort usually goes away on its own within 24 to 72 hours. You can use simple pain relievers (analgesics) to help with the pain, and supportive bras or cool compresses may ease breast soreness. However, you should seek immediate medical attention for an intense, sudden headache (thunderclap headache) or severe pain in only one breast.
Levonorgestrel Weight Gain
Acute weight gain is rare after taking a single emergency dose. Any observed fluctuation is typically minor and reversible, often due to temporary fluid retention or minor changes in appetite, rather than a lasting increase in body fat. If you experience bloating, try to moderate your salt intake and maintain regular physical activity. Note that while rare with the emergency pill, long-acting levonorgestrel methods have been linked to appetite changes in a few users.
Levonorgestrel vs Norethindrone Side Effects
Levonorgestrel and norethindrone are both progestins with comparable overall side effect profiles, but they differ in their androgenic (male hormone-like) activity. Levonorgestrel has a stronger androgenic effect than norethindrone, which means levonorgestrel may be more likely to cause acne or oily skin (seborrhea) in sensitive individuals.
- Levonorgestrel is generally better at preventing ovulation but carries a higher potential for acne, breast pain, and irregular bleeding.
- Norethindrone is frequently associated with breakthrough bleeding and headaches, and while it can have androgenic effects, they are typically milder.
- In practice, the specific dosage and pill formulation often impact real-world side effects more than the chemical structure alone.
Levonorgestrel Side Effects in Long-Term
The long-term effects are most relevant for continuous-release devices like intrauterine systems (IUS). Common experiences include irregular bleeding during the first few months, followed later by the possible cessation of periods (amenorrhea). Other effects that some users may experience are functional ovarian cysts, acne, and mood changes.
Most minor side effects will lessen after the initial adjustment period. However, serious issues are rare; you must seek immediate medical attention for pelvic pain with a fever, severe bleeding, or signs that the device might have moved or been expelled.
Possible Side Effects and Adverse Reactions
Gastrointestinal Disturbances
In addition to nausea, patients may also experience other mild digestive issues, such as indigestion (dyspepsia), abdominal cramps, or diarrhea. These symptoms are generally minor.
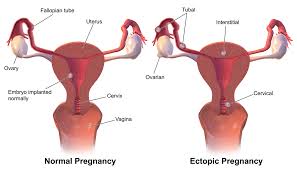
To relieve this discomfort, try having small, frequent meals and using antacids. If you have ongoing abdominal pain and there is still a possibility of pregnancy, you must be checked for an ectopic pregnancy (pregnancy outside the uterus).
Menstrual Cycle Changes
The most obvious short-term effect of taking the emergency dose is a change to your menstrual cycle. This commonly involves the next period starting a few days earlier or later, and the flow (intensity and duration) may also be different from your usual period. However, your menstrual cycle usually returns to its normal timing by the month after that.
Allergic Reactions and Skin Rashes
A true allergic reaction (hypersensitivity) is uncommon, but when it happens, it may appear as hives (urticaria), itching (pruritus), or swelling beneath the skin (angioedema).

If you experience swelling of the face, wheezing, or difficulty breathing, stop the medication immediately and seek emergency medical care. Minor rashes usually clear up well with oral antihistamines and moisturizing creams (topical emollients).
Psychological Effects Such as Mood Swings
Some people report temporary changes in emotion, such as mood swings, irritability, or short-term feelings of unhappiness (dysphoria), after taking the dose. These feelings are likely related to the rapid shifts in neurosteroids (hormones affecting the brain) caused by the medication.
These symptoms are usually temporary and will resolve on their own. However, if the symptoms are intense or continue for a long time, they should be evaluated to rule out an existing mood disorder or other possible causes.
Overdosage
Symptoms of Overdose
Because levonorgestrel has a wide therapeutic range, accidentally taking more than the recommended dose is unlikely to cause severe poisoning or toxicity.
Overdosing may, however, lead to more intense versions of the common side effects, specifically:
- Pronounced nausea, vomiting, and stomach pain.
- Temporary irregular vaginal bleeding or spotting.
- Increased headaches, dizziness, and fatigue.
Emergency Management and Supportive Care
There is no specific cure (antidote) for an overdose; treatment focuses on managing symptoms and providing support.
Initial steps include assessing the time and amount of the drug taken. Activated charcoal may be considered if a significant amount was ingested within the past hour and if appropriate for the patient. Treatment also involves controlling nausea with anti-emetic drugs and ensuring hydration and electrolyte balance. If the patient had unprotected sex, they should be evaluated for pregnancy and advised to get follow-up testing if their period is missed.
Long-Term Risks of Excessive Use
While frequent, higher-than-recommended use of the drug rarely leads to severe long-term consequences, the primary concern is endocrine disruption. This disruption can cause prolonged, unpredictable menstrual cycles and unexpected bleeding.
It's important to understand that repeatedly using emergency contraception does not substitute for a regular method of birth control. Individuals using it frequently should consider switching to a reliable ongoing method, such as a copper IUD, levonorgestrel IUS, or combined oral contraceptives. If your menstrual cycles remain erratic for over two to three months, you should seek medical advice.

Drug Interactions
Interaction with Anticonvulsants (Phenytoin, Carbamazepine)
Certain antiepileptic drugs (such as phenytoin and carbamazepine) are enzyme-inducers that speed up the liver's breakdown of levonorgestrel. This process significantly lowers the amount of levonorgestrel in the bloodstream, potentially reducing its effectiveness as an emergency contraceptive, especially when taken near the time of ovulation. For patients on these strong enzyme-inducers, clinical best practice recommends non-oral emergency contraception alternatives.
- Other medications that pose a risk include phenobarbital, primidone, topiramate, and oxcarbazepine.
- Alternatives to consider are the copper intrauterine device (IUD) or ulipristal acetate.
- It is crucial to document the patient's concomitant medications and advise them to use backup contraception.
Reduced Effectiveness with Antibiotics and Antifungals
Most common routine antibiotics do not significantly interfere with levonorgestrel effectiveness. The main exceptions are drugs that interact with the liver enzyme CYP3A:
- Rifamycin-class antibiotics (like rifampin and rifabutin) are strong inducers, meaning they dramatically reduce levonorgestrel levels and lessen its contraceptive effect.
- The antifungal griseofulvin is a weak inducer that might also reduce effectiveness.
- In contrast, azole antifungals (like ketoconazole and fluconazole) generally increase levonorgestrel levels, which does not affect efficacy but warrants monitoring for side effects.
If a patient is taking a rifamycin or griseofulvin, it is best to choose a non-oral emergency contraception method if available.
Effects of Herbal Remedies (St. Johnâs Wort)
The herbal supplement St. John’s Wort (Hypericum perforatum) is a powerful inducer of certain liver enzymes and transport proteins (CYP3A and P-glycoprotein). This action speeds up the removal of levonorgestrel from the body, resulting in lower drug availability and therefore a potential risk of contraceptive failure. The fact that it is a natural product does not mean it is safe or without strong pharmacological effects.
- These induction effects can persist for several days after the patient stops taking the herb.
- It is advised to recommend backup birth control methods or an alternative form of emergency contraception.
Guidance on Avoiding Drug Interactions
Medication reconciliation (a careful check of all prescriptions, over-the-counter products, and herbal supplements) is essential to prevent complications. If there is any question about a potential drug interaction, the safest course is to switch to an emergency contraception method that is not affected by liver enzymes.
- Specifically, review any use of enzyme-inducing medications within the last four weeks.
- When strong inducers are present, prefer the copper IUD or ulipristal acetate.
- Always educate the patient on the correct timing of the pill, how to manage vomiting, and when to perform a pregnancy test if their period is late.
Warnings and Precautions
Effectiveness Limitations Beyond 72 Hours
The effectiveness of levonorgestrel as an emergency contraceptive decreases the longer the time elapsed since unprotected intercourse. The highest protection is achieved within the first 24 hours. After 72 hours, the ability to prevent pregnancy drops significantly, and other options offer better protection in this extended timeframe. Beyond 72 hours, the copper IUD (effective for up to 5 days) or ulipristal acetate (effective for up to 120 hours) are the preferred alternatives.
Not Intended for Regular Contraceptive Use
Emergency contraception is meant for contingency situations only, not as a regular form of birth control. Frequent use can result in unpredictable menstrual cycles and a risk of lapses in pregnancy prevention. Once the emergency situation has passed, it is crucial to establish a reliable, ongoing contraceptive method.
- Recommended ongoing methods include combined oral contraceptives, progestin-only pills, implants, or IUDs.
- Also, advise on using condoms for simultaneous protection against STIs.
Risks in Women with Existing Health Conditions
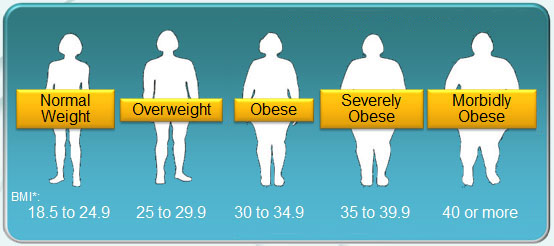
Several pre-existing medical conditions (comorbidities) necessitate caution when using levonorgestrel. Severe liver disease is a contraindication because it affects how the drug is metabolized. Conditions that impair gut function, such as malabsorption syndromes or recent bariatric surgery, can reduce oral absorption. Additionally, higher body weight may decrease the medication's effectiveness, making alternative options preferable.
- Avoid using levonorgestrel in cases of severe liver impairment.
- For those with higher BMIs, advise the use of the copper IUD or ulipristal when possible.
- While cardiovascular or metabolic risk alone is not a formal contraindication, a careful, individual risk assessment is recommended.
Importance of Follow-Up in Case of Vomiting Within 2 Hours
If vomiting occurs within two hours of taking the pill, the medication may not have been absorbed. In this case, a repeat dose is usually advised, or an alternative emergency method should be used if the vomiting persists. Any ongoing abdominal pain or a missed period requires a pregnancy test and an assessment to rule out an ectopic pregnancy. Seek immediate care for severe pain, fainting (syncope), or heavy bleeding.
Levonorgestrel Contraindications
Known Hypersensitivity to Levonorgestrel
Although allergic reactions (hypersensitivity) are rare, their occurrence prohibits any future use of the drug. Symptoms of a reaction may include hives (urticaria), swelling (angioedema), or difficulty breathing (bronchospasm). If any allergic symptoms appear, stop using the medication immediately. Standard anaphylaxis protocols should be initiated if the reaction is severe.
Existing Pregnancy
Levonorgestrel is ineffective once a pregnancy has implanted and does not cause abortion. Therefore, a known or suspected pregnancy is a contraindication for taking the emergency dose.
- Pregnancy testing should be performed if your period is more than 7 days late.
- If you experience pain or abnormal bleeding, seek an urgent medical assessment for a potential ectopic pregnancy (pregnancy outside the uterus).
Severe Liver Disease
Because the liver extensively metabolizes the drug, severe liver dysfunction is a contraindication for use. In these cases, non-hormonal alternatives should be chosen instead.
- For urgent contraceptive needs, the copper IUD should be considered.
- If contraceptive planning is complex due to liver issues, the patient should be referred for a liver specialist (hepatology) consultation.
Unexplained Vaginal Bleeding
Before starting any hormonal treatment, the cause of undiagnosed abnormal bleeding must be fully investigated. The primary goal of this diagnostic process is to eliminate complications like pregnancy issues, structural problems (e.g., fibroids), or blood clotting disorders (coagulopathy). Therefore, levonorgestrel use should be postponed until a proper gynecologic evaluation determines the underlying cause.
Careful Administration
Women with Cardiovascular Disorders
While the single, acute dose of levonorgestrel for emergency contraception is generally well tolerated, patients with pre-existing cardiovascular problems should be treated with caution. Since the systemic impact of this single dose is limited, the primary concern lies in the overall clinical context.
- It is important to evaluate baseline risks such as how well hypertension is controlled, any history of ischemic symptoms, or arrhythmias.
- For ongoing contraception, non-estrogen alternatives should be chosen to avoid potential blood pressure changes.
- Patients should be alert to and seek care for chest pain, new neurological symptoms, or a severe headache following the dose.
- When there is uncertainty, a discussion of risks versus benefits is crucial to align the treatment with the patient's heart health.
Patients with Diabetes or Obesity
Patients with metabolic conditions require individualized advice. A single emergency dose of levonorgestrel generally does not affect blood sugar control. However, body size can influence how the drug works and its overall effectiveness.
- Since increased body weight can reduce efficacy, the copper IUD or ulipristal acetate should be considered as alternatives when possible.
- Glycemic monitoring is crucial for individuals whose blood sugar has been recently unstable or who have taken steroids.
- For long-term contraception, prioritize highly effective, weight-neutral methods like IUDs or implants.
- Choosing a precise and reliable future method is key to reducing the need for emergency pills and improving contraceptive security.
History of Thromboembolic Events
Progestin-only emergency contraception (like levonorgestrel) is associated with a much lower risk of blood clots (thrombosis) than combined hormonal methods because it does not contain estrogen (ethinyl estradiol). Despite this low risk, a history of venous thromboembolism (VTE) or a clotting disorder (thrombophilia) still requires careful review.
Levonorgestrel is generally suitable for emergency use even with a history of VTE because the exposure is brief. Following the emergency use, patients should consider non-estrogen, long-acting birth control alternatives. Immediate medical evaluation is crucial for any new symptoms like leg swelling, chest pain when breathing (pleuritic pain), or shortness of breath (dyspnea).
Use in Women with Hormone-Sensitive Conditions
Conditions that can be influenced by progestins—such as migraines with aura, certain mood disorders, and hormone-sensitive cancers—require personalized guidance. Although the drug exposure from a single emergency dose is brief, caution is still advised.
- For active hormone-sensitive cancer, consult the treating specialist before using any hormonal strategy.
- For patients with a migraine with aura, monitor closely for any neurological changes, and consider a non-hormonal method for ongoing contraception.
- If significant mood swings occur, schedule a follow-up assessment if the emotional symptoms persist for more than a few days.
Important Precautions
Need for Medical Consultation if Menstruation Is Delayed
Your menstrual period timing often changes after taking this medication. If your period is delayed by more than one week from when you expected it, you need further evaluation.
- Specifically, take a pregnancy test if your period is more than seven days late.
- Seek immediate medical attention for severe abdominal pain or fainting to check for an ectopic pregnancy (a pregnancy outside the uterus).
Risks of Repeated and Frequent Use
Emergency contraception should only be used as a backup and not as a regular method of birth control. Using it repeatedly in a short period can cause irregular menstrual cycles and may decrease the reliability of protection.
- Frequent use may result in spotting, unscheduled bleeding, or delayed periods.
- While severe toxicity from repeat dosing is not expected, the predictability of your cycle declines.
- To stabilize your cycle and reduce risk, you should transition to a reliable, long-acting method of contraception.
Counseling on Future Contraceptive Planning
Counseling after the emergency event is vital to ensure the patient establishes continuous contraception, thereby preventing future urgent situations.
- Discussions should cover the effectiveness of different methods: IUDs and implants offer the highest effectiveness, while methods like pills, patches, and rings require strict, consistent use.
- Also, cover dual protection by discussing condom use to reduce the risk of STIs.
- Finally, establish a clear follow-up plan to quickly start or resume a reliable, regular contraceptive method.
Ensuring Accessibility to Safe Contraception Methods
Obstacles such as logistics, cost, and social stigma limit a person's reproductive autonomy (the freedom to make their own choices). Implementing practical solutions is therefore essential.
- Solutions include providing information on local healthcare services, telehealth options, and financial assistance programs.
- Advance provision of emergency contraception (giving it out before it's needed) should be supported where legal.
- Offering culturally competent counseling is also key to improving acceptance and consistent use of contraception.
Handling and Storage
Recommended Storage Temperature and Conditions
Keep the tablets at a controlled room temperature, ensuring they are protected from too much heat, moisture, and direct sunlight. Since bathrooms are often humid, they are not recommended for storage. The ideal temperature range is 20−25∘C (68−77∘F), though brief times between 15−30∘C (59−86∘F) are usually acceptable. To minimize exposure to the environment, keep the tablets in their original blister packaging until you are ready to use them.
Shelf Life and Stability
The drug's stability is only guaranteed up to the expiration date listed on the label if it has been stored correctly. Exposure to heat and humidity will cause the medication to degrade faster.
Always check the expiration date before giving or taking the medication yourself. Do not use the tablets if the blister packaging is damaged, or if the tablets themselves look discolored or crumbly.
Safe Disposal of Expired Medication
Never consume tablets that are expired or damaged. Proper disposal methods are important for protecting both people in the household and the environment.
- If possible, use local community drug take-back or disposal programs.
- If a take-back program is unavailable, mix the tablets with an unappealing substance (such as used coffee grounds) and seal them in a bag before placing them in the regular household trash.
- Always remove or block out any personal information on the packaging before discarding it.
Packaging and Child Safety Measures
Even though the medication is packaged in single-dose blister packs, careful management (stewardship) is critical in homes with children or individuals at risk of accidental ingestion.
- Store the medication out of sight and reach, ideally in a locked cabinet.
- Keep the tablets in their sealed blister packs until the moment of use to prevent accidental swallowing.
- Inform other household members about what the medication is for and how it is meant to be used.
i-Pill, Levonorgestrel FAQ
- How long after taking Levonorgestrel can I breastfeed?
- How long does Levonorgestrel stay in the body?
- How long does Levonorgestrel delay ovulation?
- How many Levonorgestrel pills should I take?
- How long does Levonorgestrel side effects last?
- Does Levonorgestrel cause weight gain?
- Can Levonorgestrel stop your period?
- Can Levonorgestrel delay period?
- Where can I buy Levonorgestrel?
- Can you drink alcohol after taking Levonorgestrel?
- Levonorgestrel effectiveness during ovulation?
- Can Levonorgestrel cause yeast infection?
- Does Levonorgestrel expire?
- Does Levonorgestrel work during ovulation?
- Can I take Levonorgestrel while breastfeeding?
- Does Levonorgestrel work after ovulation?
- Are Levonorgestrel pills safe?
- Are Levonorgestrel pills available in the Philippines?
- Are Levonorgestrel and Desogestrel the same?
- Are Levonorgestrel and Norgestimate the same?
- Are Levonorgestrel pills effective?
- Are Levonorgestrel and Progesterone the same?
- What are Levonorgestrel tablets used for?
- What are Levonorgestrel and Ethinyl Estradiol tablets?
- Are all Levonorgestrel pills the same?
- What are Levonorgestrel tablets?
- What are Levonorgestrel pills?
- Are all Levonorgestrel the same?
- What are Levonorgestrel and Ethinyl Estradiol tablets used for?
- What are Levonorgestrel pills used for?
- What are Levonorgestrel used for?
- Can Levonorgestrel cause bleeding?
- Can Levonorgestrel stop your period?
- Can Levonorgestrel cause weight gain?
- Can Levonorgestrel cause ectopic pregnancy?
- Can Levonorgestrel prevent pregnancy?
- Can Levonorgestrel cause early period?
- Can Levonorgestrel cause spotting?
- Can Levonorgestrel prevent implantation?
- Can Levonorgestrel cause acne?
- Can Levonorgestrel delay your period?
- Can Levonorgestrel induce periods?
- Can Levonorgestrel cause abortion?
- Can Levonorgestrel abort pregnancy?
- Can Levonorgestrel prevent pregnancy during ovulation?
- Can Levonorgestrel cause blood clots?
- How Levonorgestrel works?
- How Levonorgestrel tablet works?
- How Levonorgestrel prevent pregnancy?
- How Levonorgestrel act as contraceptive?
- How Levonorgestrel IUD works?
- How Levonorgestrel works effectiveness?
- How Levonorgestrel side effects?
- How Levonorgestrel works weight?
- How Levonorgestrel works as emergency contraception?
- How Levonorgestrel mechanism of action?
- How Levonorgestrel works time frame?
- How Levonorgestrel when to take?
- Levonorgestrel how to use?
- Levonorgestrel how many days?
- Levonorgestrel how many to take?
- Levonorgestrel what hormone?
- Levonorgestrel what does it do?
- Levonorgestrel what is it made of?
- Levonorgestrel what to avoid?
- Levonorgestrel what type of hormone?
- Levonorgestrel what does it contain?
- Levonorgestrel what to expect?
- What is Levonorgestrel and Ethinyl Estradiol?
- What does Levonorgestrel do to the body?
- When Levonorgestrel doesn’t work?
- What is Levonorgestrel tablet?
- When does Levonorgestrel start working?
- Levonorgestrel when to use?
- Levonorgestrel when ovulating?
- Levonorgestrel when breastfeeding?
- When does Levonorgestrel not work?
- When is Levonorgestrel effective?
- When is Levonorgestrel most effective?
- When can Levonorgestrel be taken?
- Which contraceptive has Levonorgestrel as progestin?
- Where to get Levonorgestrel pills?
- Which statement about Levonorgestrel requires correction?
- Which is better Levonorgestrel or Desogestrel?
- Which is better Levonorgestrel vs Norethindrone?
- Which IUD has Levonorgestrel?
- Who cannot take Levonorgestrel?
- Why Levonorgestrel tablet is used?
- Why Levonorgestrel is used?
- Why does Levonorgestrel cause bleeding?
- Why does Levonorgestrel cause weight gain?
- Why use Levonorgestrel Ethinyl Estradiol?
- Why is Levonorgestrel used instead of Progesterone?
- Why does Levonorgestrel cause acne?
- Why is Levonorgestrel contraindicated in breast cancer?
- Why does Levonorgestrel delay ovulation?
- Will Levonorgestrel work after ovulation?
- Will Levonorgestrel stop my period?
- Will Levonorgestrel work during ovulation?
- Will Levonorgestrel start my period?
- Will Levonorgestrel delay my period?
- Will Levonorgestrel cause weight gain?
- When will Levonorgestrel not work?
- Will Levonorgestrel cause acne?
How long after taking Levonorgestrel can I breastfeed?
It is generally recommended to wait a minimum of 8 hours after taking Levonorgestrel before breastfeeding. This waiting period helps reduce the concentration of the drug in breast milk, thereby minimizing the infant's exposure.
How long does Levonorgestrel stay in the body?
Levonorgestrel has a half-life of roughly 24 hours, which means it can remain in the body for around 4 to 5 days before it is completely eliminated.
How long does Levonorgestrel delay ovulation?
Levonorgestrel can postpone ovulation by approximately 5 to 7 days, based on the timing of its intake within the menstrual cycle.
How many Levonorgestrel pills should I take?
For emergency contraception, it's advised to take a single dose of 1.5 mg Levonorgestrel, or alternatively, two 0.75 mg tablets taken at the same time.
How long does Levonorgestrel side effects last?
Side effects like nausea, headaches, or irregular bleeding typically clear up within a few days, though menstrual changes might persist until the next period.
Does Levonorgestrel cause weight gain?
Weight gain is not typically a side effect of single-dose Levonorgestrel, although some users might experience temporary bloating or fluid retention.
Can Levonorgestrel stop your period?
Levonorgestrel might not entirely halt a period, but it can lead to the next menstrual cycle occurring earlier, later, or heavier than normal.
Can Levonorgestrel delay period?
Yes, Levonorgestrel can postpone the start of the next period by as much as one week, depending on when it is taken during the cycle.
Where can I buy Levonorgestrel?
Levonorgestrel is accessible over the counter at pharmacies in numerous countries, and it can additionally be ordered online from authorized medical providers.
Can you drink alcohol after taking Levonorgestrel?
Alcohol does not impact the effectiveness of Levonorgestrel, but drinking excessively may exacerbate side effects such as nausea.
Levonorgestrel effectiveness during ovulation?
Levonorgestrel is not as effective if ovulation has already taken place, since its main function is to delay or prevent ovulation.
Can Levonorgestrel cause yeast infection?
Levonorgestrel usually does not lead to yeast infections; any signs of vaginal discomfort are more likely attributed to hormonal fluctuations.
Does Levonorgestrel expire?
Yes, Levonorgestrel comes with an expiration date on the packaging and should not be used beyond that date to ensure reliable effectiveness.
Does Levonorgestrel work during ovulation?
Can I take Levonorgestrel while breastfeeding?
Yes, Levonorgestrel can be used during breastfeeding, but it's advisable to wait a few hours before nursing to minimize infant exposure.
Does Levonorgestrel work after ovulation?
Levonorgestrel is not expected to be effective once ovulation has taken place, since it cannot hinder fertilization or implantation at that point.
Are Levonorgestrel pills safe?
Levonorgestrel pills are generally regarded as safe for most women when taken as directed, although they can lead to short-term side effects like nausea, dizziness, or changes in menstruation.
Are Levonorgestrel pills available in the Philippines?
Yes, Levonorgestrel pills can be found in the Philippines, available both as emergency contraceptives and as regular contraceptive pills, and they are frequently obtainable without a prescription.
Are Levonorgestrel and Desogestrel the same?
No, Levonorgestrel and Desogestrel are distinct progestins; Levonorgestrel is frequently used in emergency contraception and intrauterine devices, whereas Desogestrel is usually found in combined oral contraceptives or progestin-only pills.
Are Levonorgestrel and Norgestimate the same?
No, Levonorgestrel and Norgestimate are separate synthetic progestins, each possessing unique pharmacological properties and applications in a range of contraceptive formulations.
Are Levonorgestrel pills effective?
Yes, Levonorgestrel pills are effective, especially when taken within 72 hours after unprotected intercourse, with effectiveness declining the longer the wait to take them.
Are Levonorgestrel and Progesterone the same?
No, Levonorgestrel is a man-made progestin, whereas Progesterone is a hormone that occurs naturally in the body, though both interact with progesterone receptors.
What are Levonorgestrel tablets used for?
Levonorgestrel tablets are mainly used for emergency contraception to avert pregnancy following unprotected intercourse or contraceptive failure, and in certain instances as a component of continuous contraceptive methods.
What are Levonorgestrel and Ethinyl Estradiol tablets?
Levonorgestrel and Ethinyl Estradiol tablets are a type of combined oral contraceptive that includes both a synthetic progestin and estrogen. They work together to prevent ovulation and help regulate the menstrual cycle.
Are all Levonorgestrel pills the same?
No, Levonorgestrel pills differ in dosage, formulation, and intended purpose, such as emergency contraception compared to standard daily contraceptives.
What are Levonorgestrel tablets?
Levonorgestrel tablets are oral medications that contain the synthetic progestin Levonorgestrel. They are primarily used to prevent pregnancy in emergency situations or as part of contraceptive methods.
What are Levonorgestrel pills?
Levonorgestrel pills are medications formulated to prevent pregnancy, used either as single-dose emergency contraceptives or as daily contraceptive pills combined with other hormones.
Are all Levonorgestrel the same?
No, Levonorgestrel can be produced in various doses, delivery systems, and combinations, which means that not every product containing it has the same application or effect.
What are Levonorgestrel and Ethinyl Estradiol tablets used for?
Levonorgestrel and Ethinyl Estradiol tablets are commonly prescribed for regular contraception, regulating menstrual cycles, and at times, for addressing hormonal imbalances or conditions like acne.
What are Levonorgestrel pills used for?
Levonorgestrel pills are utilized to avert unintended pregnancy, either as emergency contraception following unprotected intercourse or as a component of long-term contraceptive methods.
What are Levonorgestrel used for?
Levonorgestrel is utilized for pregnancy prevention, found in emergency contraceptive pills, intrauterine devices, and specific hormonal contraceptive methods.
Can Levonorgestrel cause bleeding?
Yes, Levonorgestrel can lead to irregular bleeding or spotting, a common side effect following use, particularly with emergency contraceptive doses.
Can Levonorgestrel stop your period?
Levonorgestrel typically does not completely stop a period, but it can change the timing or flow of the upcoming menstrual cycle.
Can Levonorgestrel cause weight gain?
Levonorgestrel is generally not linked to considerable weight gain, although some users might experience short-term bloating or fluid retention.
Can Levonorgestrel cause ectopic pregnancy?
Levonorgestrel does not directly lead to ectopic pregnancy; however, in rare instances when contraception fails, a pregnancy may happen and carries the same risk of being ectopic as any other pregnancy.
Can Levonorgestrel prevent pregnancy?
Yes, Levonorgestrel can prevent pregnancy by postponing ovulation and blocking fertilization, particularly when taken quickly after unprotected intercourse.
Can Levonorgestrel cause early period?
Yes, Levonorgestrel can lead to an early period by affecting the usual hormonal balance and timing of the menstrual cycle.
Can Levonorgestrel cause spotting?
Yes, experiencing spotting or irregular bleeding is a common side effect after using Levonorgestrel, particularly with emergency contraception.
Can Levonorgestrel prevent implantation?
Levonorgestrel mainly functions by inhibiting or postponing ovulation, and it is not deemed effective in stopping implantation after fertilization has taken place.
Can Levonorgestrel cause acne?
Acne is not a typical side effect of Levonorgestrel; however, hormonal fluctuations in some instances may lead to skin breakouts.
Can Levonorgestrel delay your period?
Yes, Levonorgestrel can postpone the start of the next period by a few days, based on when it is taken during the cycle.
Can Levonorgestrel induce periods?
Levonorgestrel does not consistently trigger periods, but it might lead to earlier or more intense bleeding as a short-term hormonal response.
Can Levonorgestrel cause abortion?
Can Levonorgestrel abort pregnancy?
No, Levonorgestrel cannot terminate an existing pregnancy; it solely works by preventing ovulation or fertilization if taken promptly.
Can Levonorgestrel prevent pregnancy during ovulation?
Levonorgestrel is less effective if ovulation has already taken place, since its primary function is to delay or prevent ovulation.
Can Levonorgestrel cause blood clots?
The likelihood of blood clots associated with a single emergency dose of Levonorgestrel is exceptionally low, significantly lower than that of long-term combined hormonal contraceptives.
How Levonorgestrel works?
Levonorgestrel functions by postponing ovulation, thickening cervical mucus to obstruct sperm movement, and modifying the uterine lining to lower the likelihood of fertilization.
How Levonorgestrel tablet works?
Levonorgestrel tablets primarily prevent pregnancy by halting or postponing ovulation, which makes it challenging for sperm to reach or fertilize an egg.
How Levonorgestrel prevent pregnancy?
Levonorgestrel works to prevent pregnancy by either inhibiting or delaying ovulation and also by decreasing sperm penetration through the cervical mucus.
How Levonorgestrel act as contraceptive?
Levonorgestrel functions as a contraceptive by preventing ovulation, altering the cervical mucus to deter sperm, and establishing an environment that is not conducive to fertilization.
How Levonorgestrel IUD works?
A Levonorgestrel intrauterine device (IUD) delivers small doses of hormone straight into the uterus, enhancing cervical mucus, reducing the thickness of the endometrium, and occasionally inhibiting ovulation to avoid pregnancy.
How Levonorgestrel works effectiveness?
Levonorgestrel works best when taken promptly after unprotected sex, showing the highest success rates within 24 hours, which gradually decline over the subsequent 72 hours.
How Levonorgestrel side effects?
Levonorgestrel side effects can include nausea, headache, dizziness, breast tenderness, fatigue, and alterations in menstrual bleeding, which typically resolve within a few days.
How Levonorgestrel works weight?
Levonorgestrel itself does not have a direct impact on weight; however, some users might notice temporary bloating or fluid retention, which can create the feeling of weight fluctuation.
How Levonorgestrel works as emergency contraception?
Levonorgestrel functions as emergency contraception by postponing or inhibiting ovulation, thickening cervical mucus, and lowering the likelihood of fertilization when taken quickly after unprotected intercourse.
How Levonorgestrel mechanism of action?
The way Levonorgestrel works includes the suppression or delay of ovulation, blocking sperm from penetrating cervical mucus, and changing the endometrium to prevent fertilization.
How Levonorgestrel works time frame?
Levonorgestrel works best when taken within 72 hours after unprotected sex, showing the highest success rate if administered within 24 hours.
How Levonorgestrel when to take?
Levonorgestrel should be taken as soon as possible after unprotected intercourse, ideally within the first 24 hours to ensure maximum effectiveness.
Levonorgestrel how to use?
Levonorgestrel is administered orally as one single 1.5 mg tablet, or two 0.75 mg tablets taken simultaneously, without the necessity for continued dosing.
Levonorgestrel how many days?
Levonorgestrel is most effective when taken within 3 days (72 hours) following unprotected intercourse, although taking it sooner offers greater protection.
Levonorgestrel how many to take?
The typical dose is one 1.5 mg tablet, or alternatively, two 0.75 mg tablets taken together as one single dose.
Levonorgestrel what hormone?
Levonorgestrel is a synthetic progestin hormone that replicates the effects of natural progesterone in the body.
Levonorgestrel what does it do?
Levonorgestrel prevents pregnancy by inhibiting ovulation, thickening cervical mucus, and modifying the uterine lining to reduce the chances of fertilization.
Levonorgestrel what is it made of?
Levonorgestrel is a synthetic version of the natural hormone Progesterone, specifically formulated to deliver contraceptive benefits.
Levonorgestrel what to avoid?
While using Levonorgestrel, try not to postpone intake beyond 72 hours and be mindful of specific medications such as anticonvulsants or St. John’s Wort, which may lessen its effectiveness.
Levonorgestrel what type of hormone?
Levonorgestrel is a synthetic progestogen that falls under the category of progestins used in contraceptive drugs.
Levonorgestrel what does it contain?
Levonorgestrel tablets include the active hormone Levonorgestrel, often accompanied by inactive ingredients like lactose, starch, or magnesium stearate.
Levonorgestrel what to expect?
After taking Levonorgestrel, users might experience mild side effects such as nausea, fatigue, irregular bleeding, and alterations in the timing of their next menstrual period.
What is Levonorgestrel and Ethinyl Estradiol?
Levonorgestrel and Ethinyl Estradiol is a combined oral contraceptive that includes a synthetic progestin and estrogen to inhibit ovulation and manage menstrual cycles.
What does Levonorgestrel do to the body?
Levonorgestrel modifies reproductive hormone functions by inhibiting ovulation, increasing the thickness of cervical mucus, and reducing the receptiveness of the uterine lining to implantation.
When Levonorgestrel doesn’t work?
Levonorgestrel may be ineffective if ovulation has already taken place, if it is taken more than 72 hours after unprotected intercourse, or if drug interactions diminish its effectiveness.
What is Levonorgestrel tablet?
A Levonorgestrel tablet is an oral contraceptive that contains the synthetic progestin Levonorgestrel. It is utilized for emergency contraception or is part of certain birth control methods.
When does Levonorgestrel start working?
Levonorgestrel begins to take effect as soon as it is absorbed, usually within a few hours, with peak effectiveness reached when taken promptly after unprotected intercourse.
Levonorgestrel when to use?
Levonorgestrel is intended for use as emergency contraception within 72 hours following unprotected intercourse, with the best results achieved when taken within the first 24 hours.
Levonorgestrel when ovulating?
Levonorgestrel is not as effective if ovulation has already taken place, since its primary function is to delay or prevent ovulation prior to the release of the egg.
Levonorgestrel when breastfeeding?
Levonorgestrel can be used during breastfeeding, but it is recommended to wait at least 8 hours before nursing to reduce the infant's exposure.
When does Levonorgestrel not work?
Levonorgestrel is ineffective if taken after fertilization and implantation, or if ovulation has already taken place at the time of intake.
When is Levonorgestrel effective?
Levonorgestrel is most effective when taken within 72 hours following unprotected intercourse, achieving the highest success rate when taken as soon as possible.
When is Levonorgestrel most effective?
Levonorgestrel works best within the first 24 hours following unprotected sex, with its effectiveness diminishing gradually as time passes.
When can Levonorgestrel be taken?
Levonorgestrel can be taken at any point during the menstrual cycle following unprotected intercourse, as long as it is within 72 hours.
Which contraceptive has Levonorgestrel as progestin?
Several contraceptives feature Levonorgestrel as the progestin, such as emergency contraceptive pills, combined oral contraceptives, and intrauterine devices like Mirena and Skyla.
Where to get Levonorgestrel pills?
Levonorgestrel pills are available at pharmacies, clinics, and from licensed online medical providers in numerous countries.
Which statement about Levonorgestrel requires correction?
The mistaken belief is that Levonorgestrel induces abortion; however, it actually prevents pregnancy from occurring in the first place and has no effect after implantation has happened.
Which is better Levonorgestrel or Desogestrel?
The decision between Levonorgestrel and Desogestrel is guided by clinical requirements; Levonorgestrel is typically utilized for emergency contraception and IUDs, whereas Desogestrel is more frequently found in daily progestin-only pills.
Which is better Levonorgestrel vs Norethindrone?
Both are effective progestins, but Levonorgestrel is preferred for emergency contraception and IUDs, while Norethindrone is commonly used in progestin-only pills and hormone therapy.
Which IUD has Levonorgestrel?
Intrauterine devices like Mirena, Skyla, Liletta, and Kyleena use Levonorgestrel as the active hormone.
Who cannot take Levonorgestrel?
Levonorgestrel should be avoided by anyone with a known allergy to the drug, unexplained vaginal bleeding, severe liver disease, or those who are already pregnant.
Why Levonorgestrel tablet is used?
Levonorgestrel tablets are utilized to prevent pregnancy following contraceptive failure or unprotected intercourse, offering a reliable and effective method of emergency contraception.
Why Levonorgestrel is used?
Levonorgestrel is utilized for emergency contraception, regular contraception in specific formulations, and as the active hormone in particular intrauterine devices.
Why does Levonorgestrel cause bleeding?
Levonorgestrel may lead to bleeding as it interferes with the natural hormonal balance, resulting in alterations to the endometrial lining and irregular shedding.
Why does Levonorgestrel cause weight gain?
Levonorgestrel usually does not result in substantial weight gain, but fluid retention and hormonal shifts can occasionally cause temporary bloating or slight weight changes.
Why use Levonorgestrel Ethinyl Estradiol?
Why is Levonorgestrel used instead of Progesterone?
Levonorgestrel is commonly preferred over Progesterone as it is a reliable synthetic progestin with consistent bioavailability and high contraceptive efficacy.
Why does Levonorgestrel cause acne?
Levonorgestrel can trigger acne in certain users because of its androgenic effects, which may activate sebaceous gland activity and result in breakouts.
Why is Levonorgestrel contraindicated in breast cancer?
Levonorgestrel is not recommended for those with breast cancer as it is a hormone that may stimulate hormone-sensitive tumors, potentially exacerbating the condition.
Why does Levonorgestrel delay ovulation?
Levonorgestrel postpones ovulation by inhibiting the surge of luteinizing hormone, which is essential for the ovary to release an egg.
Will Levonorgestrel work after ovulation?
Levonorgestrel is not likely to be effective after ovulation since its main function is to prevent or delay ovulation prior to fertilization happening.
Will Levonorgestrel stop my period?
Levonorgestrel typically does not prevent a period, but it can change its timing, flow, or lead to spotting before the anticipated period.
Will Levonorgestrel work during ovulation?
Levonorgestrel is less effective during ovulation, as the egg may have already been released, which restricts its capacity to prevent pregnancy.
Will Levonorgestrel start my period?
Levonorgestrel can cause early bleeding or spotting, but it does not consistently result in a regular menstrual period.
Will Levonorgestrel delay my period?
Yes, Levonorgestrel can postpone the next menstrual period by a few days, depending on when it is taken during the cycle.
Will Levonorgestrel cause weight gain?
Significant weight gain is rare with Levonorgestrel, although mild bloating or temporary fluid retention may occur.
When will Levonorgestrel not work?
Levonorgestrel will not be effective if taken after implantation has occurred, if ovulation has already occurred, or if interactions with other drugs diminish its efficacy.
Will Levonorgestrel cause acne?
Levonorgestrel can lead to acne in certain individuals because of its mild androgenic properties, although not everyone will experience this side effect.