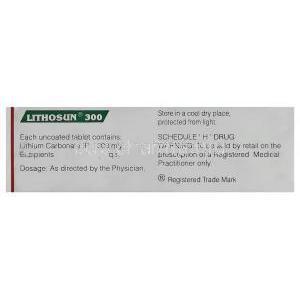
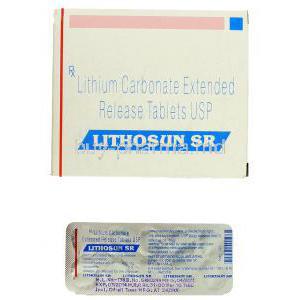
Lithium
Uses
Lithosun is used in the treatment of mood disorders such as, mania, bipolar disorder, hypomania and depression.
How it Works
Lithosun is known as a psychiatric medicine. Lithosun works by affecting sodium transport in the nerve cells.Lithosun reduces the intensity and frequency of mood swings. It affects the amount of some chemical substances present in the brain, and it may also affect the way that nerve cells respond to some of the chemical substances.
Common Side effects
Patients who take Lithosun may suffer from such side effects; Acne,
Changes in taste,
Slightly shaky hands,
Pruritis affecting the skin,
Dry hair ,
Hair loss,
Slurred speech,
Uncoordinated body movements,
Nausea,
Increased white blood cell count,
Memory impairment,
Enlarged thyroid gland,
Skin rash,
Increased thirst,
Weight gain,
Polyuria,
Diarrhoea
Changes in taste,
Slightly shaky hands,
Pruritis affecting the skin,
Dry hair ,
Hair loss,
Slurred speech,
Uncoordinated body movements,
Nausea,
Increased white blood cell count,
Memory impairment,
Enlarged thyroid gland,
Skin rash,
Increased thirst,
Weight gain,
Polyuria,
Diarrhoea