Introduction to Vancomycin
Overview of Vancomycin as a Glycopeptide Antibiotic
Vancomycin is a powerful glycopeptide antibiotic reserved for serious bacterial infections. It exerts potent bactericidal activity against Gram-positive organisms and is often deployed when other antimicrobials fail. This unique status makes it a cornerstone in treating resistant pathogens.
Historical Background and Discovery
First isolated in the 1950s from Amycolatopsis orientalis, vancomycin quickly became a pivotal therapy. Originally regarded as a “last chance” drug, its use expanded during the rise of methicillin-resistant bacteria. Decades later, it continues to retain importance in hospital and intensive care settings.
Role in Modern Medicine and Classification as a Last-Resort Antibiotic
Today, vancomycin is classified as a last-resort antibiotic. It is employed when standard agents, such as beta-lactams, are ineffective or contraindicated. This designation underscores both its therapeutic value and the need for judicious use to mitigate resistance.
Composition and Formulations of Vancomycin
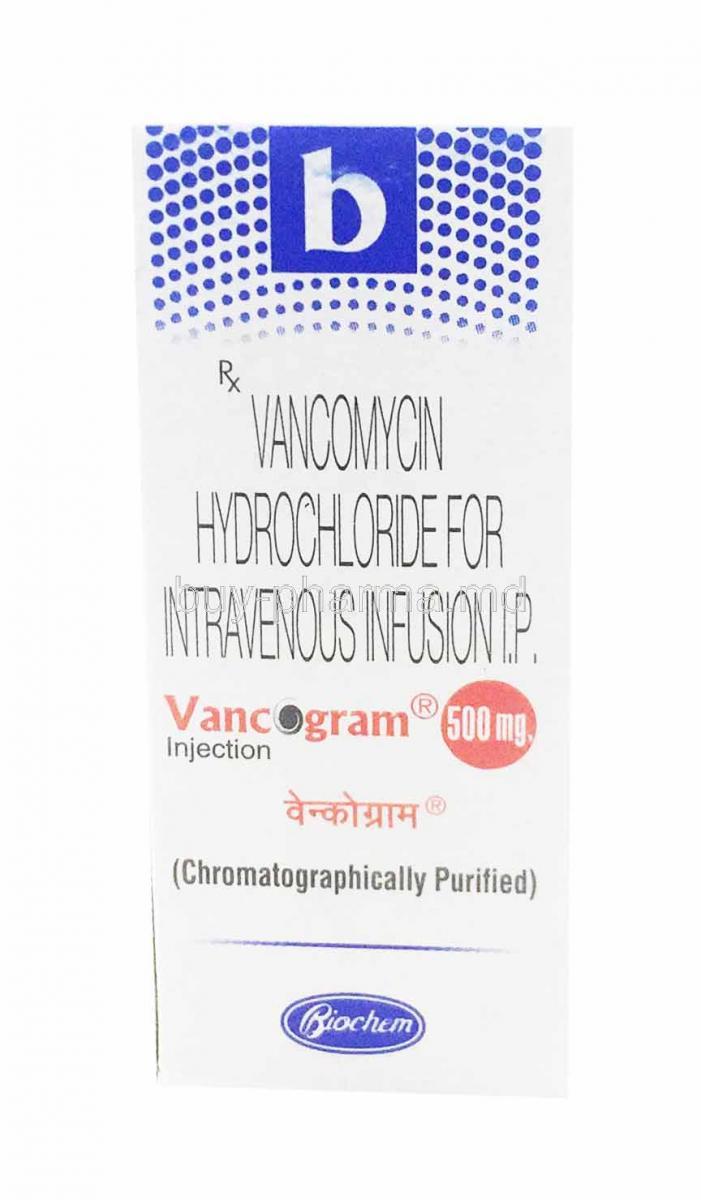
Active Pharmaceutical Ingredient: Vancomycin Hydrochloride
The primary compound is vancomycin hydrochloride, a crystalline form designed for both oral and intravenous administration. Its molecular structure enables it to bind with precision to bacterial targets.
Available Dosage Forms
- Intravenous infusion powder for reconstitution
- Oral capsules for localized gastrointestinal infections
- Oral solution for patients unable to swallow solid forms
Brand Names and Generic Variations
Marketed under various brand names worldwide, vancomycin is also widely available as a cost-effective generic. Despite brand differences, the pharmacological activity remains consistent.
Excipients and Formulation Differences Across Preparations
Inactive ingredients vary across formulations, including stabilizers, fillers, and buffers. These excipients influence stability, absorption, and patient tolerability.
Mechanism of Action: How Vancomycin Works
Inhibition of Bacterial Cell Wall Synthesis
Vancomycin disrupts bacterial survival by halting cell wall synthesis. Without a rigid wall, bacteria cannot maintain structural integrity, leading to cell death.
Binding to D-alanyl-D-alanine Residues
Its mechanism involves binding tightly to D-alanyl-D-alanine residues of peptidoglycan precursors. This prevents cross-linking and weakens bacterial defense systems.
Effect on Gram-Positive Bacteria, Including MRSA
Vancomycin shows strong activity against Gram-positive organisms. Notably, it is indispensable in combating methicillin-resistant Staphylococcus aureus (MRSA), which is unresponsive to many other antibiotics.
Development of Resistance: VRE
Emergence of vancomycin-resistant enterococci (VRE) poses a global health challenge. These strains alter their target binding sites, reducing vancomycin’s effectiveness and complicating therapy.
Approved Medical Uses of Vancomycin
- Severe Gram-positive bacterial infections resistant to standard therapy
- MRSA bloodstream and tissue infections
- Endocarditis caused by susceptible organisms
- Bacteremia and septicemia requiring intensive therapy
- Pneumonia, particularly in hospitalized patients
- Osteomyelitis and bone-related infections
- Skin and soft tissue infections of resistant origin
- Meningitis and central nervous system infections
- Clostridioides difficile–associated diarrhea treated with oral vancomycin
Off-Label Uses of Vancomycin
- Surgical prophylaxis for patients allergic to beta-lactams
- Management of febrile neutropenia
- Treatment of infections in immunocompromised patients (HIV, transplant, chemotherapy)
- Enterocolitis caused by Gram-positive bacteria other than C. difficile
- Prophylaxis in prosthetic valve surgery
- Intrathecal administration for refractory CNS infections
Dosage and Administration of Vancomycin
Standard Dosing Guidelines for Adults
Doses are typically calculated by weight and renal function, ensuring optimal therapeutic effect while minimizing toxicity.
Oral Dosing for C. difficile Infections
Oral vancomycin is reserved for localized gastrointestinal treatment, with standard regimens spanning 10 to 14 days.
Intravenous Dosing for Systemic Infections
IV vancomycin is infused over at least 60 minutes to reduce infusion-related reactions. Dose adjustments are frequent based on infection severity and patient status.
Individualized Dosing Based on Renal Function
Because vancomycin is primarily excreted renally, patients with impaired kidney function require careful dose adjustments and close monitoring.
Therapeutic Drug Monitoring
Monitoring includes trough serum levels or AUC/MIC ratios. Proper monitoring prevents both under-dosing and dangerous accumulation.
Administration Techniques
- Infusion duration of 60 minutes or longer
- Avoidance of rapid IV push to prevent hypotension and flushing
- Use of central lines for prolonged therapy to prevent phlebitis
Dose Adjustment in Hepatic or Renal Impairment
While hepatic impairment has minimal impact, renal dysfunction significantly alters clearance, necessitating individualized regimens.
Administration in Special Populations
Elderly Patients
Aging kidneys reduce vancomycin clearance. Elderly individuals face heightened risks of nephrotoxicity and ototoxicity, making vigilant monitoring essential.
Pregnant Women and Nursing Mothers
Vancomycin crosses the placenta, though teratogenicity remains low. It is excreted in breast milk, warranting caution and medical guidance during lactation.
Pediatric Patients
Neonates and children metabolize vancomycin differently. Premature infants, in particular, are vulnerable to toxicity, necessitating precise dosing and serum monitoring.
Side Effects of Vancomycin
Common Side Effects
- Infusion-related reactions, notably “red man syndrome” with flushing and rash
- Phlebitis at infusion site
- Nausea, vomiting, and gastrointestinal upset when administered orally
- Mild skin rash and irritation
Serious and Rare Adverse Effects
- Nephrotoxicity: acute kidney injury requiring frequent monitoring
- Ototoxicity: potential irreversible hearing loss, particularly with prolonged therapy
- Hypersensitivity reactions: ranging from urticaria to full anaphylaxis
- Hematologic toxicity: rare neutropenia or thrombocytopenia
- Severe dermatologic reactions: Stevens-Johnson syndrome or toxic epidermal necrolysis
Drug Interactions with Vancomycin
Interaction with Aminoglycosides: Increased Nephrotoxicity
When vancomycin is administered alongside aminoglycosides such as gentamicin or tobramycin, the risk of nephrotoxicity rises substantially. Both drug classes exert deleterious effects on renal tubular cells, and their concurrent use demands vigilant monitoring of kidney function.
Concurrent Use with Loop Diuretics: Enhanced Ototoxicity
Loop diuretics, including furosemide, may amplify vancomycin-induced ototoxicity. Patients exposed to this combination face an increased likelihood of hearing impairment, tinnitus, or vestibular disturbances. Careful dosing and routine auditory evaluations are recommended when these agents must be used together.
Interaction with Other Nephrotoxic Agents
Nephrotoxic drugs such as amphotericin B, cyclosporine, and certain chemotherapeutic agents can exacerbate vancomycin’s renal risks. Combining these therapies requires a delicate balance of therapeutic benefit against potential kidney injury.
Compatibility Issues with Other IV Medications
Vancomycin may not be physically compatible with several intravenous agents. Precipitation or inactivation may occur when mixed in the same infusion line. To avoid adverse outcomes, vancomycin should often be administered separately or with dedicated infusion lines.
Impact on Therapeutic Monitoring with Other Antibiotics
When vancomycin is used in multi-drug regimens, particularly with beta-lactams or rifampin, interpreting serum drug levels and therapeutic endpoints becomes more complex. Monitoring protocols must account for overlapping toxicity and synergistic or antagonistic effects.
Warnings and Important Precautions
Risk of Rapid Infusion and "Red Man Syndrome"
Infusing vancomycin too quickly can precipitate flushing, erythema, and hypotension, collectively termed "red man syndrome." This reaction is not typically allergic but is distressing and preventable by extending infusion times.
Need for Therapeutic Drug Monitoring
Vancomycin has a narrow therapeutic window. Regular monitoring of trough levels or AUC/MIC ratios ensures efficacy while minimizing nephrotoxicity and ototoxicity. Skipping this step can jeopardize patient safety.
Importance of Renal Function Monitoring
Because the drug is excreted renally, kidney function tests should be performed frequently. Any sign of rising serum creatinine or declining clearance warrants immediate dose adjustment.
Avoidance of Unnecessary Prolonged Therapy
Long-term use promotes resistance, including the emergence of vancomycin-resistant enterococci. Therapy should be limited to evidence-based indications and discontinued promptly when no longer necessary.
Monitoring for Superinfection and Clostridioides difficile Overgrowth
Broad-spectrum antibiotics like vancomycin may disrupt normal flora, leading to opportunistic infections. Vigilance for Clostridioides difficile or fungal overgrowth is crucial during extended courses.
Contraindications of Vancomycin
Known Hypersensitivity to Vancomycin
Patients with documented allergy to vancomycin or its components must avoid use. Re-exposure may trigger severe dermatologic or systemic reactions.
History of Severe Allergic Reaction to Glycopeptides
Cross-reactivity with other glycopeptides may occur. Individuals with a history of severe hypersensitivity should only receive vancomycin under strict medical supervision, if at all.
Careful Administration Considerations
Patients with Pre-existing Renal Impairment
Reduced clearance in kidney disease heightens toxicity risks. Tailored dosing and frequent monitoring are essential to prevent irreversible renal damage.
Patients with Pre-existing Hearing Loss or Concurrent Ototoxic Drug Use
Those with baseline auditory deficits or receiving ototoxic medications require extra caution. Baseline and periodic audiometric assessments are advisable.
Patients with Inflammatory Bowel Disease
Oral vancomycin can occasionally be absorbed systemically in patients with severe colitis or mucosal injury. This may elevate plasma concentrations and toxicity risk.
Patients Receiving Prolonged Therapy
Long-term administration may cause hematologic abnormalities such as neutropenia or thrombocytopenia. Regular complete blood counts are recommended for these patients.
Overdosage of Vancomycin
Signs and Symptoms of Overdose
- Worsening nephrotoxicity with acute kidney injury
- Ototoxicity leading to partial or permanent hearing loss
- Profound hypotension and cardiovascular instability
Emergency Management
Management is primarily supportive. Prompt discontinuation of the drug, intravenous hydration, and close monitoring of vital functions form the cornerstone of care. Hemodialysis, though variably effective, may assist in reducing circulating drug levels in critical cases.
Monitoring and Dose Adjustment Following Overdose
Serial serum levels guide recovery and inform subsequent dosing. Future therapy, if unavoidable, must be accompanied by meticulous monitoring to prevent recurrence.
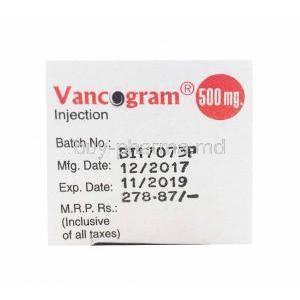
Storage and Handling Precautions
Recommended Storage Conditions
Vancomycin vials and oral solutions should be stored at controlled room temperature, away from moisture and direct light. Refrigeration may be required for certain liquid preparations after reconstitution.
Reconstitution Guidelines for Intravenous Powder
Powdered vancomycin should be reconstituted with sterile water and further diluted before infusion. Proper technique ensures stability and minimizes contamination risks.
Stability After Dilution and Reconstitution
Solutions remain stable for a limited period, often 24 hours at room temperature or up to several days under refrigeration. Stability guidelines vary with concentration and diluent.
Handling Precautions for Healthcare Providers
Healthcare workers should employ aseptic technique during preparation and administration. Gloves and protective equipment reduce occupational exposure risks.
Safe Disposal of Unused or Expired Medication
Leftover or expired vancomycin must be disposed of according to institutional protocols for hazardous pharmaceutical waste. This prevents environmental contamination and accidental misuse.
Vancomycin FAQ
- What is the drug vancomycin used for?
- Is vancomycin the strongest antibiotic?
- What is the most serious side effect of vancomycin?
- Is vancomycin a penicillin?
- What to avoid while taking vancomycin?
- What bacteria does vancomycin not treat?
- Is vancomycin better than amoxicillin?
- How does vancomycin make you feel?
- What happens when you stop taking vancomycin?
- Does vancomycin treat pneumonia?
- What infections need vancomycin?
- What antibiotic is stronger than vancomycin?
- What happens if vancomycin doesn't work?
- What is another name for vancomycin?
- How long does vancomycin stay in your system?
- Can vancomycin make you tired?
- What to monitor while taking vancomycin?
- What are two infections that vancomycin can treat?
- What antibiotic can replace vancomycin?
- What bacteria are killed by vancomycin?
- Is co-amoxiclav the same as vancomycin?
- What antibiotic is stronger than vancomycin for C diff?
- What bacteria are resistant to vancomycin?
- Does vancomycin make you poop more?
- How long can you be on vancomycin for C diff?
- How many days is vancomycin given?
- What level of vancomycin is needed for pneumonia?
- Can vancomycin cause hearing loss?
What is the drug vancomycin used for?
Vancomycin is prescribed for infections resulting from bacteria by either eliminating the bacteria or hindering their growth.
Is vancomycin the strongest antibiotic?
Yes
What is the most serious side effect of vancomycin?
Toxic epidermal necrolysis
Is vancomycin a penicillin?
No
What to avoid while taking vancomycin?
- Amikacin
- Aminoglycosides
- Bile acid sequestrants
- NSAIDS
What bacteria does vancomycin not treat?
VRE
Is vancomycin better than amoxicillin?
Yes
How does vancomycin make you feel?
It can cause itching and rashes.
What happens when you stop taking vancomycin?
Your illness might not be entirely cured, and the bacteria could develop resistance to antibiotics.
Does vancomycin treat pneumonia?
Yes
What infections need vancomycin?
- Endocarditis
- Peritonitis
- Infections of the lungs, skin, blood, and bones
What antibiotic is stronger than vancomycin?
Linezolid
What happens if vancomycin doesn't work?
The dosage of vancomycin may be raised to 2 grams per day.
What is another name for vancomycin?
Vancocin
How long does vancomycin stay in your system?
4 to 6 hours
Can vancomycin make you tired?
Yes
What to monitor while taking vancomycin?
Serum creatinine, vancomycin levels, and MRSA PCR screens.
What are two infections that vancomycin can treat?
The management of blood poisoning (septicemia), inflammation of the heart lining (endocarditis), skin and skin structure infections (such as cellulitis), bone infections (osteomyelitis), and lower respiratory tract infections (like pneumonia).
What antibiotic can replace vancomycin?
- Clindamycin
- Cephalexin
- Ciprofloxacin
- Metronidazole
- Ceftriaxone
- Levofloxacin
What bacteria are killed by vancomycin?
- Staphylococcus aureus (including strains to methicillin)
- Staphylococcus epidermidis (including strains that are resistant to multiple medications).
Is co-amoxiclav the same as vancomycin?
Yes
What antibiotic is stronger than vancomycin for C diff?
Fidaxomicin
What bacteria are resistant to vancomycin?
Enterococci germs
Does vancomycin make you poop more?
Yes
How long can you be on vancomycin for C diff?
10 to 14 days
How many days is vancomycin given?
7-10 days
What level of vancomycin is needed for pneumonia?
15-20 mg/L
Can vancomycin cause hearing loss?
No