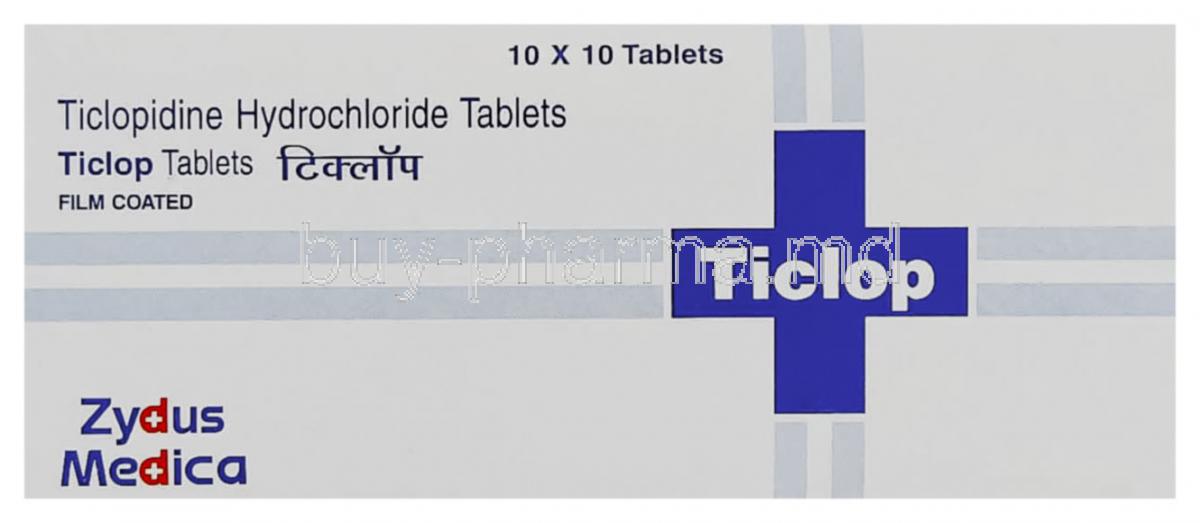
Introduction to Ticlop (Ticlopidine)
Overview of Ticlop and its Clinical Significance
Ticlop, known generically as ticlopidine, is a potent antiplatelet agent designed to reduce the risk of thrombotic events. It has been a cornerstone therapy for patients who require effective platelet inhibition, particularly when other options such as aspirin are unsuitable.
By impeding platelet aggregation, ticlopidine helps safeguard against the formation of clots that can obstruct blood flow to vital organs, reducing the risk of ischemic stroke and other vascular complications.
History of Development and Approval Status
Ticlopidine was introduced in the late 20th century as one of the first agents in its class. Its approval in multiple countries marked a pivotal advancement in the prevention of cerebrovascular and cardiovascular events. Although newer agents like clopidogrel have gained prominence, ticlopidine remains clinically relevant in specific cases.
Comparison with Other Antiplatelet Drugs
- Aspirin: Widely used but less effective in certain patients due to resistance or intolerance.
- Clopidogrel: A newer analogue with fewer hematologic risks but higher cost.
- Ticlopidine: Particularly valuable when aspirin is contraindicated or poorly tolerated.
Composition and Formulation
Active Ingredient: Ticlopidine Hydrochloride
The therapeutic component of Ticlop is ticlopidine hydrochloride, which exerts antiplatelet effects through irreversible receptor inhibition.
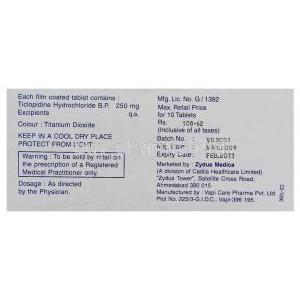
Available Strengths and Dosage Forms
Ticlop is most commonly formulated as oral tablets, typically in 250 mg strength, facilitating precise dosing for long-term therapy.
Inactive Ingredients and Excipients
Excipients may include cellulose derivatives, magnesium stearate, and other stabilizers that ensure tablet integrity and bioavailability.
Mechanism of Action: How Ticlopidine Works
Inhibition of ADP-Mediated Platelet Aggregation
Ticlopidine selectively blocks the adenosine diphosphate (ADP) pathway responsible for platelet aggregation, disrupting clot formation at the earliest stage.
Effect on Platelet Membrane Receptors
By antagonizing the P2Y12 receptor, ticlopidine diminishes platelet adhesion and cross-linking, reducing thrombus formation.
Irreversible Binding and Duration of Antiplatelet Action
Each dose exerts an irreversible effect on circulating platelets. As a result, platelet function recovery requires the production of new platelets, usually taking 7–10 days after discontinuation.
Approved Medical Uses of Ticlopidine
Prevention of Thrombotic Stroke
Ticlopidine is indicated for reducing the risk of recurrent ischemic stroke in patients with a history of stroke or transient ischemic attacks (TIAs).
Secondary Prevention of Cardiovascular Events
It lowers the incidence of vascular events in high-risk populations, including those with established atherosclerotic disease.
Use in Patients Intolerant to Aspirin
For individuals unable to tolerate aspirin due to hypersensitivity or gastrointestinal complications, ticlopidine provides a viable and effective alternative.
Off-Label Uses of Ticlopidine
Coronary Stent Placement
Ticlopidine has been employed in preventing stent thrombosis following coronary angioplasty procedures.
Peripheral Arterial Disease
It can aid in preventing ischemic episodes and improve blood flow in patients with peripheral vascular disease.
Hemodialysis Shunt Patency
By reducing thrombus formation, ticlopidine helps maintain the patency of arteriovenous shunts in dialysis patients.
Atrial Fibrillation
In patients unsuitable for anticoagulation therapy, ticlopidine may serve as an alternative antiplatelet strategy.
Dosage and Administration Guidelines
Standard Adult Dosing Recommendations
The usual dose is 250 mg taken orally twice daily. Clinical monitoring is required, especially during the first three months of treatment.
Loading Dose vs. Maintenance Dose
While loading doses are not always necessary, maintenance therapy is critical for sustained platelet inhibition.
Duration of Therapy Based on Indication
Treatment duration varies; for stroke prevention, long-term therapy is often advised, whereas post-stent use may be time-limited.
Missed Dose Instructions
If a dose is missed, patients should take it as soon as remembered unless it is close to the next scheduled dose. Doubling up is not recommended.
Administration with Food
Ticlopidine is best taken with meals to reduce gastrointestinal side effects and enhance absorption.
Side Effects of Ticlopidine
Overview of Possible Adverse Reactions
Ticlopidine, while effective, can produce hematologic, gastrointestinal, and dermatologic adverse events that warrant vigilance.
Hematologic Effects
- Neutropenia and agranulocytosis
- Thrombocytopenia
- Rare cases of aplastic anemia
Dermatologic and Allergic Reactions
Patients may experience rash, pruritus, or hypersensitivity responses.
Gastrointestinal Disturbances
Nausea, diarrhea, and abdominal discomfort are relatively common and usually mild.
Common Side Effects
- Nausea and dyspepsia
- Diarrhea
- Skin rash and pruritus
- Dizziness or mild headache
Serious and Rare Adverse Effects
- Thrombotic thrombocytopenic purpura (TTP)
- Aplastic anemia and pancytopenia
- Severe hepatic dysfunction with jaundice
Drug Interactions
- Anticoagulants: Heightened risk of bleeding when combined with warfarin or heparin.
- Other Antiplatelets: Enhanced bleeding tendency with aspirin or clopidogrel.
- CYP450 Metabolism: Potential pharmacokinetic interactions with hepatic enzyme inhibitors or inducers.
- Alcohol and NSAIDs: Increased gastrointestinal bleeding risk.
Contraindications
- Hypersensitivity to ticlopidine
- History of hematologic disorders such as agranulocytosis
- Active bleeding including peptic ulcer or intracranial hemorrhage
- Severe hepatic impairment
Warnings and Important Precautions
- Hematologic Toxicity: Risk of life-threatening agranulocytosis, aplastic anemia, or TTP.
- Monitoring: Regular complete blood counts are essential during the first 3 months.
- Hepatic Impairment: Use with caution in patients with liver disease.
- Surgical Considerations: Increased risk of perioperative bleeding; discontinuation prior to surgery may be necessary.
Careful Administration
Monitoring Requirements During the First 3 Months of Therapy
The initial phase of ticlopidine therapy requires stringent monitoring. Complete blood counts should be performed at regular intervals, typically every two weeks for the first three months. This vigilant approach helps detect early signs of neutropenia, agranulocytosis, or thrombocytopenia before they evolve into severe complications.
Caution in Patients with Renal Impairment
Renal dysfunction may alter the clearance of ticlopidine. While specific dose adjustments are not always mandated, patients with moderate to severe impairment require careful clinical observation. Monitoring renal function alongside hematologic parameters reduces the risk of accumulation and toxicity.
Use in Patients with Increased Bleeding Risk
Ticlopidine amplifies bleeding tendencies. Individuals with pre-existing coagulopathies, gastrointestinal ulcers, or recent surgical procedures must be managed cautiously. Temporary discontinuation may be required before invasive interventions to minimize hemorrhagic events.
Special Population Considerations
Administration in Elderly Patients
The elderly often exhibit altered pharmacokinetics and enhanced susceptibility to adverse drug reactions.
- Dose Adjustment: Standard dosing is usually maintained, but clinical discretion is advised in frail or multi-morbid patients.
- Hematologic Risk: Older adults have an increased propensity for neutropenia and anemia, warranting closer laboratory surveillance.
Administration in Pregnant Women and Nursing Mothers
Limited clinical data exist regarding ticlopidine use during pregnancy. Animal studies suggest potential teratogenic effects, yet definitive human data are lacking.
- Pregnancy: Ticlopidine should be prescribed only if the potential maternal benefit clearly outweighs fetal risk.
- Breastfeeding: The drug is excreted in breast milk. Nursing mothers are generally advised to avoid use or discontinue breastfeeding to prevent neonatal exposure.
Administration in Children
The safety and efficacy of ticlopidine in pediatric populations remain unestablished. Due to the risk of severe hematologic and hepatic side effects, its use in children is not recommended.
Overdosage of Ticlopidine
Symptoms of Overdose
Excessive ingestion can provoke severe bleeding, mucocutaneous hemorrhage, and markedly prolonged clotting times. Other manifestations may include dizziness, weakness, and gastrointestinal upset.
Emergency Management and Supportive Care
Treatment of overdose is largely supportive. Prompt hospitalization is warranted, with continuous monitoring of hematologic indices and coagulation parameters.
Role of Platelet Transfusion
Since ticlopidine irreversibly inhibits platelet aggregation, transfusion of functional platelets may be necessary in life-threatening bleeding episodes. Adjunctive measures such as intravenous fluids and hemodynamic support should also be employed.
Handling and Storage Precautions
Recommended Storage Conditions
Ticlopidine tablets should be stored at controlled room temperature, ideally between 20°C and 25°C. Excessive humidity and direct sunlight must be avoided to preserve drug stability.
Shelf Life and Expiration Considerations
Each batch carries a specific expiration date. Use beyond this timeframe is discouraged, as potency and safety cannot be guaranteed.
Safe Handling Instructions for Healthcare Providers
Healthcare professionals should handle ticlopidine with care. Gloves may be recommended during large-scale dispensing to reduce dermal exposure, especially for individuals with known hypersensitivity.
Disposal Guidelines for Unused Medication
Unused or expired tablets should not be discarded in household waste or wastewater. Instead, they should be returned to authorized collection points or disposed of according to local pharmaceutical waste regulations.