Introduction to Tacrocip (Tacrolimus)
Overview of Tacrocip brand and generic classification
Tacrocip is a pharmaceutical preparation containing tacrolimus, a potent immunosuppressive compound. Classified under calcineurin inhibitors, this medicine is employed to attenuate immune hyperactivity in specific medical conditions. It exists both as a branded formulation and as a generic equivalent, ensuring accessibility to patients across diverse healthcare systems.
Historical background and development of tacrolimus
Discovered in the late 1980s from the soil bacterium Streptomyces tsukubaensis, tacrolimus was originally identified for its antifungal properties. Its exceptional immunosuppressive effect soon positioned it as a critical advancement in transplant medicine, reducing graft rejection rates significantly. Since then, it has gained global recognition for both systemic and topical therapeutic applications.
Therapeutic category: calcineurin inhibitors and immunosuppressants
Tacrolimus belongs to the therapeutic category of calcineurin inhibitors, a class that modulates immune responses by halting T-cell activation. By doing so, it preserves transplanted organs, minimizes autoimmune attacks, and alleviates inflammatory skin conditions resistant to conventional therapy.
Composition and Formulations
Active ingredient: tacrolimus
The cornerstone of Tacrocip is tacrolimus, a macrolide lactone with highly selective immunosuppressive activity.
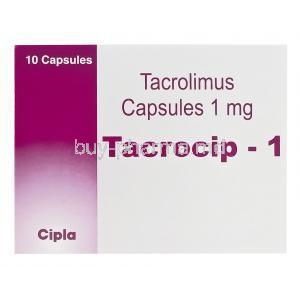
Available strengths and dosage forms (capsules, ointment, injection)
- Oral capsules in various strengths, commonly 0.5 mg, 1 mg, and 5 mg
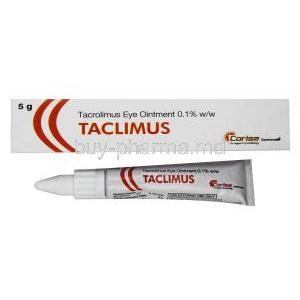
- Topical ointments for dermatological conditions
- Intravenous injection for acute and hospital-based therapy
Inactive ingredients and excipients
Excipients vary by formulation but may include stabilizers, emulsifiers, and protective agents designed to ensure bioavailability and product stability.
Branded vs. generic versions
Both branded and generic tacrolimus products are widely available. Generics undergo stringent bioequivalence testing, offering similar efficacy and safety profiles at more affordable price points.
Mechanism of Action: How Tacrolimus Works
Role of tacrolimus as a calcineurin inhibitor
Tacrolimus suppresses calcineurin, a pivotal enzyme in T-cell activation, thereby interrupting the cascade of immune signaling.
Immunosuppressive mechanism at the cellular level
At the molecular level, tacrolimus binds to FK-binding protein (FKBP-12), forming a complex that inhibits calcineurin phosphatase. This blockade prevents transcription of interleukin-2 and other cytokines essential for immune proliferation.
Effect on T-lymphocyte activation and cytokine production
The downstream effect is diminished T-lymphocyte activation, reduced cytokine release, and a lower likelihood of immune-mediated graft rejection or inflammatory flare-ups.
Comparison with other immunosuppressants (cyclosporine, sirolimus)
Compared to cyclosporine, tacrolimus demonstrates greater potency with fewer cosmetic side effects such as hirsutism and gum hypertrophy. Sirolimus, another immunosuppressant, acts synergistically but has distinct mechanisms, often used in combination therapy.
Approved Medical Uses
Prevention of organ transplant rejection (kidney, liver, heart, lung)
Tacrocip is a mainstay for transplant patients, safeguarding vital organs by reducing the risk of acute and chronic rejection.
Treatment of graft-versus-host disease (GVHD) after bone marrow transplantation
In bone marrow recipients, tacrolimus is a frontline agent for preventing and treating GVHD, a condition where donor immune cells attack the recipient’s tissues.
Management of atopic dermatitis and eczema (topical formulations)
Topical tacrolimus is approved for moderate to severe atopic dermatitis, particularly where corticosteroids are unsuitable. It alleviates itching, redness, and inflammation with long-term tolerability.
Off-Label Uses of Tacrocip (Tacrolimus)
Use in autoimmune conditions (lupus nephritis, myasthenia gravis)
Tacrolimus is often prescribed in difficult-to-treat autoimmune disorders where standard regimens fall short.
Role in inflammatory bowel disease (Crohn’s disease, ulcerative colitis)
Although not universally approved, tacrolimus has shown efficacy in inducing remission in refractory cases of inflammatory bowel disease.
Use in dermatological conditions (psoriasis, vitiligo, lichen planus)
Its topical formulation has expanded into conditions such as vitiligo and lichen planus, where it modulates aberrant skin immune activity.
Neurological and experimental therapeutic indications
Emerging research explores tacrolimus in neurological disorders, leveraging its neuroprotective properties in conditions like amyotrophic lateral sclerosis.
Dosage and Administration
Standard dosing guidelines for transplant patients
Dosage depends on the transplanted organ, weight, and clinical response, typically starting higher post-transplant and tapering to maintenance levels.
Dosing for dermatological and autoimmune conditions
Topical ointment is applied in thin layers, while oral dosing for autoimmune disorders requires careful titration to balance efficacy and toxicity.
Adjustments for renal and hepatic impairment
Patients with impaired kidney or liver function require lower doses and stringent monitoring to avoid accumulation and adverse effects.
Administration routes: oral, topical, intravenous
Tacrolimus is administered through multiple routes depending on the clinical scenario. Each requires strict adherence to avoid underdosing or overdosing.
Importance of therapeutic drug monitoring
Regular measurement of blood trough levels is crucial to ensure therapeutic effect while minimizing toxicities.
Side Effects of Tacrocip
Common Side Effects
- Headache, tremors, dizziness
- Nausea, vomiting, diarrhea
- Insomnia and sleep disturbances
- Hypertension, hyperglycemia
Serious Side Effects
- Heightened susceptibility to infections
- Nephrotoxicity and hepatotoxicity
- Neurological events such as seizures or confusion
- Increased risk of malignancies, including skin cancer and lymphoma
Warnings and Important Precautions
Risk of opportunistic infections and malignancies
Long-term tacrolimus therapy is associated with elevated risks of opportunistic infections and certain cancers, necessitating vigilant follow-up.
Need for regular monitoring (blood levels, kidney and liver function)
Continuous assessment of drug levels and organ function is indispensable to optimize therapy and reduce risks.
Sun exposure precautions to reduce cancer risk
Patients are advised to avoid excessive ultraviolet exposure, utilize sun protection, and monitor for skin changes to mitigate malignancy risk.
Avoidance of live vaccines during therapy
Because of its immunosuppressive action, tacrolimus users should not receive live vaccines, as this may provoke severe infections or diminished efficacy.
Contraindications
Known hypersensitivity to tacrolimus or excipients
Patients with a documented history of hypersensitivity to tacrolimus or any component within its formulation must not receive this therapy. Hypersensitivity may present as severe dermatological eruptions, respiratory difficulty, or systemic anaphylaxis.
Concomitant systemic use with cyclosporine
The simultaneous systemic administration of cyclosporine and tacrolimus is contraindicated due to overlapping mechanisms of action. Their combined use may amplify nephrotoxicity and enhance immunosuppression beyond safe thresholds.
Patients with uncontrolled infections
In individuals battling active, uncontrolled infections, tacrolimus use is discouraged. Suppression of immune defenses in such circumstances may precipitate life-threatening complications.
Use in patients with known malignancies without monitoring
Tacrolimus may accelerate the progression of malignancies. In patients with known neoplastic conditions, administration without rigorous oncological monitoring poses unacceptable risks.
Careful Administration and Monitoring
Monitoring blood concentrations of tacrolimus
Precise measurement of trough blood levels is essential. Subtherapeutic dosing risks graft rejection, whereas supratherapeutic exposure predisposes patients to toxicity.
Regular evaluation of renal and hepatic function
Periodic assessment of renal clearance and hepatic enzymes is mandated. Tacrolimus-associated nephrotoxicity and hepatotoxicity can emerge insidiously, requiring early detection.
Blood pressure and blood sugar monitoring
Hypertension and hyperglycemia are frequent metabolic consequences. Monitoring enables timely pharmacological or dietary interventions.
Precautions in switching brands or formulations
Variability in bioavailability across branded and generic formulations necessitates heightened vigilance when transitioning. Clinicians should re-assess serum concentrations and clinical stability during such changes.
Special Population Considerations
Administration to Elderly Patients
- Increased susceptibility to nephrotoxicity due to age-related decline in renal reserve
- Greater likelihood of polypharmacy, leading to interaction risks
- Necessity for cautious dose adjustments and close clinical observation
Administration to Pregnant Women
Tacrolimus crosses the placenta and may influence fetal development. Documented risks include intrauterine growth restriction and preterm birth.
- Potential teratogenic effects necessitate individualized assessment
- Close monitoring of maternal blood levels and fetal growth parameters is advised
Administration to Nursing Mothers
Excretion into breast milk introduces the potential for neonatal exposure.
- Risk–benefit assessment is crucial when considering continuation of breastfeeding
- In cases of continued use, infants should be monitored for immunosuppressive effects
Administration to Children
Pediatric patients exhibit different pharmacokinetics, requiring tailored dosing regimens. Growth, development, and organ function must be carefully monitored throughout therapy.
Drug Interactions
Interaction with CYP3A4 inhibitors and inducers (e.g., ketoconazole, rifampin)
CYP3A4 inhibitors significantly increase tacrolimus plasma levels, elevating toxicity risk. Conversely, CYP3A4 inducers decrease levels, endangering therapeutic efficacy.
Interactions with nephrotoxic and hepatotoxic drugs
Concurrent administration with other nephrotoxic or hepatotoxic drugs amplifies organ injury. Examples include aminoglycoside antibiotics and amphotericin B.
Food and grapefruit juice interactions
Grapefruit juice impedes tacrolimus metabolism, increasing systemic exposure. Consistency in food intake relative to dosing is recommended to minimize variability in absorption.
Impact on vaccine efficacy and safety
As an immunosuppressant, tacrolimus diminishes vaccine responses. Live vaccines should be avoided during therapy to prevent uncontrolled viral replication.
Overdosage and Toxicity
Clinical presentation of tacrolimus overdose
Symptoms may include profound tremors, seizures, acute renal failure, and severe hypertension. Gastrointestinal disturbances and electrolyte imbalances are common.
Immediate management strategies
No specific antidote exists. Initial measures involve cessation of dosing, gastric decontamination if appropriate, and intensive supportive care.
Supportive treatment and role of hemodialysis
Hemodialysis is generally ineffective due to high protein binding. Supportive measures, including correction of metabolic abnormalities, remain the cornerstone of management.
Handling and Storage Precautions
Recommended storage conditions for capsules, ointments, and injections
Capsules and ointments should be stored at controlled room temperature, away from moisture and direct light. Injections must be kept under refrigeration, as per manufacturer’s guidelines.
Safe handling guidelines for healthcare professionals
Healthcare personnel should employ gloves and protective measures to minimize dermal contact. Accidental exposure may result in local irritation or systemic absorption.
Disposal instructions for unused or expired medication
Expired or unused tacrolimus should be discarded in accordance with pharmaceutical waste protocols. Flushing into wastewater systems should be avoided to prevent environmental contamination.